Upgrading to CRT Has Big Impact on HFrEF Patients With High RV Pacing Burden
The findings from BUDAPEST CRT Upgrade will likely change guidelines, experts predict.
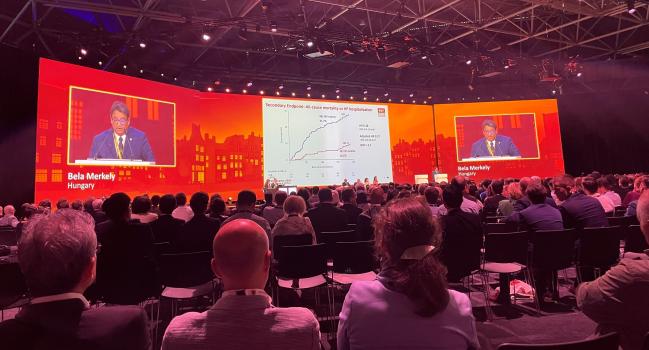
AMSTERDAM, the Netherlands—Among patients with heart failure with reduced ejection fraction (HFrEF), a previously implanted pacemaker or ICD, and a significant RV pacing burden, upgrading to a cardiac resynchronization therapy defibrillator (CRT-D) provides much better clinical outcomes than continuing with standard ICD therapy, the randomized BUDAPEST CRT Upgrade study shows.
Patients who were upgraded to CRT-D had a significantly lower rate of a primary composite endpoint of HF hospitalization, all-cause mortality, or less than a 15% reduction in LV end-systolic volume by 1 year (32.4% vs 78.9%), with a number needed to treat of just 2.2, according to Béla Merkely, MD, PhD (Semmelweis University Heart and Vascular Center, Budapest, Hungary).
LV end-systolic and end-diastolic volumes decreased to a greater extent in the upgrade group, with larger improvements also seen in LVEF, he reported here at the European Society of Cardiology Congress 2023. The findings were published simultaneously online in the European Heart Journal.
“Overall, HFrEF patients with a pacemaker or ICD should be strictly followed in clinical practice,” Merkely said, “and in those with intermittent or permanent right ventricular pacing, a CRT upgrade should be performed immediately without postponing the procedure to a later date to avoid or reduce the risk of further adverse events such as mortality, heart failure hospitalization, or left ventricular remodeling.”
Aldo Maggioni, MD (ANMCO Research Center of the Italian Association of Hospital Cardiologists, Florence, Italy), who moderated a press conference at which Merkely discussed the trial, told TCTMD that “the results are very clear in favor of the upgrade.”
He expressed skepticism about the magnitude of the observed benefit, but said “there is clear evidence that including CRT in the treatment strategy of these patients can provide some beneficial effect.”
And that’s likely to impact guidelines, although it’s unclear what the strength of any recommendation based on the results of this one trial might be, Maggioni said.
Merkely also foresees these results influencing recommendations: “This is the way to go in the future, and I hope very much that this study can clearly change the guideline at the European Society of Cardiology.”
The BUDAPEST CRT Upgrade Trial
Merkely noted that about 30% of patients with conventional pacemakers or ICDs will develop LV systolic dysfunction stemming from intraventricular dyssynchrony related to RV pacing, and that in turn can lead to HF hospitalizations and adverse clinical outcomes.
In patients with HFrEF and a pacemaker or ICD, the impact of upgrading to a CRT-D device—which involves placement of an extra LV lead—on hard clinical outcomes hasn’t been established in a randomized trial. That lack of data has led to changing recommendations for CRT upgrade over the years in both US and European guidelines. And in practice, Merkely said, most candidates for a CRT upgrade either have the procedure deferred or don’t get it at all.
BUDAPEST CRT Upgrade, conducted at 17 sites across seven countries, is the first randomized trial powered for hard endpoints to explore the impact of an upgrade in HFrEF patients with a previously implanted pacemaker or ICD and intermittent or permanent RV pacing. The study included 360 patients (mean age 73 years; 89% men) who had an RV pacing rate of at least 20% over the last 90 days and a paced QRS complex ≥ 150 ms.
Most of the patients (69%) had a pacemaker, and the rest a standard ICD. They were randomized 3:2 to receive a CRT-D upgrade or to undergo no procedure or receive an ICD. In the control group, patients who already had an ICD either received no intervention or received a CRT-D upgrade with the CRT-D function turned off.
Mean LVEF at baseline was 25%. The average RV pacing rate prior to enrollment was 85% in the CRT-D upgrade group and 88% in the control group.
The primary composite endpoint was markedly reduced in patients who received a CRT-D upgrade by 1 year (adjusted OR 0.11; 95% CI 0.06-0.19). The effect was consistent across various subgroups, including in patients who had atrial fibrillation, who made up 56% of the trial population.
There was always a question mark whether CRT is working in atrial fibrillation or not, and this study really nicely [demonstrated] that the patients with chronic atrial fibrillation, permanent atrial fibrillation, could have a benefit. Béla Merkely
“There was always a question mark whether CRT is working in atrial fibrillation or not, and this study really nicely [demonstrated] that the patients with chronic atrial fibrillation, permanent atrial fibrillation, could have a benefit,” Merkely said during a discussion after his presentation.
Among secondary endpoints, the upgrade also lowered the rate of a composite of all-cause mortality or HF hospitalization (10.2% vs 31.7%; adjusted HR 0.27; 95% CI 0.16-0.47), with a number needed to treat of 4.7. The risk of all-cause mortality alone was not significantly affected (adjusted HR 0.52; 95% CI 0.23-1.19), but HF hospitalizations were reduced (adjusted HR 0.24; 95% CI 0.13-0.44).
Echocardiographic outcomes improved with the CRT-D upgrade as well, with greater drops in LV end-systolic volume (by 50.5 vs 1.9 mL) and LV end-diastolic volume (by 40.9 vs 1.9 mL) and a larger increase in LVEF (by 11% vs 1.2%).
The CRT-D upgrade was safe, with successful procedures seen in 98.0% of the upgrade group and 100% of the control group. Though the rate of procedure- or device-related serious adverse events was higher in the upgrade group (12.3% vs 7.8%), spontaneous ventricular tachycardia or fibrillation was less frequent (0.5% vs 14.5%).
‘Highly Convincing’ Results
Serving as a discussant after Merkely’s presentation, Cecilia Linde, MD (Karolinska University Hospital, Stockholm, Sweden), pointed out that many patients receiving RV pacing have been upgraded to CRT-D based on evidence of symptomatic improvement but without solid evidence of an effect on hard outcomes.
“Therefore, the BUDAPEST CRT Upgrade trial, which is powered for outcome, is extremely important,” she said.
There are some limitations, including the long enrollment time (influenced by the COVID-19 pandemic), the open-label design, some crossovers, and loss of some echocardiographic data. Although the primary endpoint might seem unusual, she added, it’s the same one used in the BLOCK HF trial published more than a decade ago.
Overall, “we have highly convincing outcome results in favor of CRT,” Linde said, pointing out the significant LV reverse remodeling accompanied by a reduction in ventricular arrhythmias and the consistency across subgroups.
“Upgrading to CRT-D from RV pacing improves outcome in pacing-induced cardiomyopathy,” she concluded. “Early [upgrading] to CRT may prevent a patient with left ventricular dysfunction to develop heart failure. So this will be a next step. Organization of device follow-up must be optimized to detect pacing-induced cardiomyopathy. And the result, in my opinion, will probably affect guidelines.”
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Merkely B, Hatala R, Wranicz JK, et al. Upgrade of right ventricular pacing to cardiac resynchronisation therapy in heart failure: a randomised trial. Eur Heart J. 2023;Epub ahead of print.
Disclosures
- BUDAPEST CRT Upgrade was funded by grants from Boston Scientific, the National Research Development and Innovation Fund of Hungary, and the European Union.
- Merkely reports receiving research contracts from Abbott, AstraZeneca, Biotronik, Boehringer Ingelheim, Boston Scientific, Bristol Myers Squibb, CSL Behring, Daiichi Sankyo, the Duke Clinical Research Institute, Eli Lilly, Medtronic, Novartis, Terumo, and Vifor Pharma and having other relationships with Abbott, AstraZeneca, Biotronik, Boehringer Ingelheim, CSL Behring, Daiichi Sankyo, the Duke Clinical Research Institute, Medtronic, and Novartis.
- Linde reports receiving research grants from the Swedish Heart-Lung Foundation, Stockholm City Council, and Swedish Academy of Science, and speaker honoraria from AstraZeneca, Bayer, Novartis, Vifor, Medtronic, Abbott, Boehringer Ingelheim, and Impulse Dynamics.





Comments