Viability Testing Fails to Find HF Patients Who’d Benefit From PCI in REVIVED-BCIS2
PCI didn’t improve prognosis or LV recovery in ischemic cardiomyopathy no matter what viability looked like at baseline.
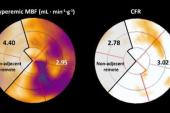
Photo Credit: Adapted from Perera D. Revascularization in LV systolic dysfunction: revived or dead? Presented at: TCT 2022. Boston, MA.
NEW ORLEANS, LA—No matter what the viability testing shows, there is no significant benefit to PCI when compared with optimal medical therapy in patients with impaired left ventricular function and extensive coronary artery disease, according to a new analysis of REVIVED-BCIS2 study.
PCI did not improve prognosis or LV recovery regardless of the viability characteristics at baseline, nor were the presence of dysfunctional-yet-viable myocardial segments associated with patient prognosis or recovery. The deep dive into the trial, which was presented earlier this week at the American College of Cardiology/World Congress of Cardiology (ACC/WCC) 2023 meeting, throws into question some long-held views about hibernating myocardium, say investigators.
“I think it challenges it, because we had come to use viability tests as our prospective marker of hibernation,” said lead REVIVED-BCIS2 investigator Divaka Perera, MD (King’s College London, England), during a packed featured clinical research session. “Of course, that’s predicated on an assumption that we can pick the parts of the ventricle that recover, [and thus] the patient who is going to have LV recovery. Using the very metrics we currently use, we’ve shown that [viability] doesn’t predict LV recovery. I think we need to challenge the paradigm. Hibernation, as we’ve known and used it, doesn’t seem to be useful in clinical practice anymore.”
As to whether viability testing should be used to identify patients who might benefit from revascularization, Perera said the answer is an unequivocal no. “There is absolutely no evidence from this or from the STICH data that it predicts a group of patients who benefit,” he said.
Characterization by viability assessment doesn’t allow us to select a group of patients who would benefit from PCI over medical therapy. Divaka Perera
Sunil Rao, MD (NYU Langone Medical Center, New York), agreed that the analysis challenges current concepts and definitions of hibernating myocardium.
“The whole idea behind hibernating myocardium is that it’s dysfunctional, yet viable in that revascularization or reestablishing blood flow should make it normal again,” Rao told TCTMD. “And the observational data bear that out. There is Raymond Kim’s paper in the New England Journal of Medicine years ago that showed there was an association with revascularization and improved function in these dysfunctional segments with 50% or less scar. The remarkable thing about REVIVED is that they basically tested that directly.”
Rao said physicians are struggling with if or when to revascularize patients with extensive stable coronary artery disease and impaired LV ejection fraction. While the 5-year results of STICH didn’t show any benefit of CABG over medical therapy, a survival advantage with surgery emerged by 10 years. In REVIVED, PCI did not reduce the incidence of death from any cause or hospitalization for heart failure compared with guideline-directed medical therapy. There is also ISCHEMIA and COURAGE to factor in, as well
“If the idea is to revascularize just to improve the ejection fraction, I don’t think you’re going to achieve that,” Rao said. “If they have symptoms, then that’s probably the reason to revascularize. The question is, should we be testing for viability to help guide those decisions? I kind of agree with Divaka [Perera]—routine use of viability testing isn’t supported by these data. The question then becomes, in whom should we use viability testing? I don’t think we know the answer to that.”
Can’t Find That ‘Goldilocks’ Zone
In presenting the new results, Perera, like Rao, said observational data had led many to believe that viability testing was a useful instrument to identify those who would benefit from revascularization. Patients who had viable myocardium—which was defined as yes/no in these early studies—appeared to fare much better with revascularization than those without viable myocardium. Data from the STICH trial, however, challenged the viability hypothesis, with investigators reporting the presence of viable myocardium didn’t predict the benefit of CABG surgery in patients with ischemic cardiomyopathy.
Given these conflicting findings, the investigators set out to better understand the importance of viable myocardium in the REVIVED cohort, including whether viability predicted event-free survival, the response to PCI or optimal medical therapy, and whether it was associated with left ventricular recovery. In turn, they also wanted to assess if left ventricular recovery was associated with event-free survival. The majority of patients underwent viability testing with cardiac magnetic resonance (CMR) imaging while dobutamine stress echocardiography (DSE) was used in roughly 20% of patients.
In viability testing, myocardial segments were initially classified as normokinetic or dysfunctional, with the dysfunctional segments further classified as dysfunctional-viable, which is a correlate of hibernating myocardium, or nonviable. The viable segments were defined as those with contractile reserve on DSE or CMR late-gadolinium enhancement ≤ 25%.
If I get an MRI and it shows me a ton of scar in the left ventricle, then I’m worried about that patient. Kevin Bainey
Regardless of treatment allocation, patients with more viable myocardium were less likely to die or be hospitalized for heart failure, whereas the presence of more dysfunctional-yet-viable myocardium was not significantly associated with event-free survival. Similarly, there was no relationship between the extent of dysfunctional-yet-viable segments and LV recovery, although LV recovery itself was associated with the risk of death or heart failure hospitalizations. Among those who had increases in ejection fraction above the median change, there was a 38% lower risk of the primary endpoint when compared with those who had less LV recovery (P = 0.029).
Scar burden, too, tracked with outcomes: for each 10% increase in scar volume, there was an 18% higher risk of death or heart failure hospitalizations (HR 1:18; 95% CI 1.04-1.33).
“If you characterize the myocardium in terms of scar, or the extent of nonviable myocardium, it is highly predictive of prognosis and the likelihood of LV recovery, and that’s independent of baseline left ventricular ejection fraction,” said Perera.
In terms of the effects of PCI versus guideline-directed medical therapy (GDMT) in the trial, there was no difference in outcomes by treatment allocation based on the amount of hibernating myocardium or scar burden. Similarly, the extent of scar or dysfunctional-yet-viable myocardium segments at baseline was not useful for predicting whether PCI or GDMT would improve LV recovery across tertiles of patients with dysfunctional-yet-viable segments at baseline.
“Characterization by viability assessment doesn’t allow us to select a group of patients who would benefit from PCI over medical therapy,” said Perera. “There isn’t a ‘Goldilocks’ zone that we identified.”
Benefits of Identifying Myocardial Scar
Speaking with TCTMD, Rao said that use of CMR to identify scar burden can be helpful because “it’s clearly prognostic” and can help inform conversations with the patient, and possibly help them be more adherent to medication, as an example. “Beyond that, I think it’s a really confusing time,” he said. Myocardial scar can be reflection of previous cardiovascular events, the extent of their CAD, and likely the duration of their disease. “In a way, it’s not surprising that scar in and of itself is not prognostically important,” he said. “What is surprising is that it didn’t seem to matter if you got medical therapy or PCI.”
Kevin Bainey, MD (Mazankowski Alberta Heart Institute/University of Alberta, Edmonton, Canada), who wasn’t involved in the study, said the prognostic implications of scar is an important finding, one that makes sense biologically. “As a clinician, if I get an MRI and it shows me a ton of scar in the left ventricle, then I’m worried about that patient,” he said. “It might push me towards thinking about an ICD [implantable cardioverter-defibrillator] for prevention. This could change a clinician’s thought process about how to best risk stratify that patient long term.”
One of the limitations, he said, is that researchers used stress echo and CMR as opposed to PET imaging, which is what most people use for viability assessments.
Perera doesn’t think viability testing should be discarded entirely but stressed that it shouldn’t be focused on dysfunctional segments to identify patients who would benefit from PCI or those with the potential for LV recovery. “Instead, in those very viability tests that we do is embedded useful information: scar and nonviable myocardium,” he said, noting that irreversible injury remains a powerful predictor of prognosis. “Whether we can use this to risk-stratify patients better or apply it to ICD therapy, and so on, will need to be tested in future trials.”
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Perera D, on behalf of the REVIVED-BCIS2 investigators. Effect of myocardial viability, functional recovery, and PCI on clinical outcomes in the REVIVED-BCIS2 trial. Presented at: ACC/WCC 2023. March 4, 2023. New Orleans, LA.
Disclosures
- Perera reports no relevant conflicts of interest.



Comments