VIVA: No Difference Between TAVI and SAVR for Small Aortic Annuli
With only 2-year follow-up it’s challenging to interpret long-term outcomes, says Yousif Ahmad.
SAN FRANCISCO. CA—In patients with severe aortic stenosis and small aortic annuli, SAVR and TAVI result in similar 2-year outcomes for mortality, stroke, and cardiac rehospitalization events, the international VIVA study shows.
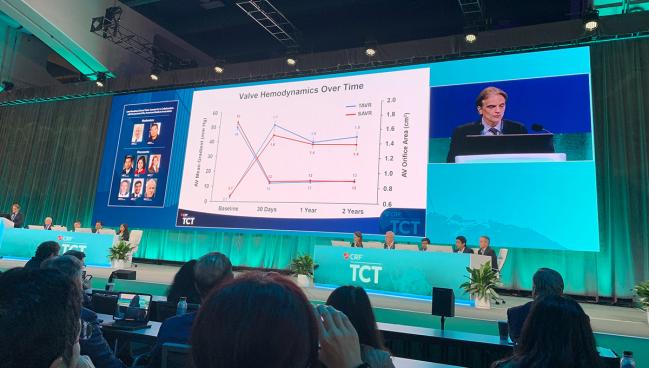
Unlike many aortic stenosis trials, VIVA distinguishes itself by having a population of more than 90% women, essentially because they were more likely than men to meet criteria for true small aortic annulus, said Josep Rodés-Cabau, MD, PhD (Laval University/Quebec Heart & Lung Institute, Canada), presenting the late-breaking trial in a press conference here at TCT 2023.
“The findings suggest that these two therapies could be a valid alternative for treating patients with aortic stenosis and small aortic annulus,” he said.
In addition to the 2-year clinical outcomes, there were no differences between TAVI and SAVR groups in the incidence of severe prosthesis patient mismatch (PPM) or moderate-severe aortic regurgitation (AR) at 60 days despite some nonrandomized studies suggesting that valve hemodynamics tend to be superior with TAVI in patients with small aortic annuli. In terms of early outcomes, those randomized to surgery had higher rates of major/life-threatening bleeding and atrial arrhythmias than those randomized to TAVI.
“I think with 2-year data it’s challenging to interpret any clinical implications when we're looking at valve function. I honestly think even 5-year data is going to be too short. What we want to know is what's happening to these valves a decade out,” Yousif Ahmad, MD, PhD (Yale University School of Medicine, New Haven, CT), who wasn’t involved in the study, said in the press conference.
As the authors acknowledge in the VIVA manuscript, simultaneously published in Circulation, the study was underpowered. Ahmad noted that the rate of PPM was double in the surgical arm compared with the TAVI arm, which is consistent with prior data in the field. “I suspect that with a larger sample size that would be statistically significant,” he added.
VIVA was stopped when only 50% of the expected population had been enrolled, which Rodés-Cabau said was related to slow recruitment as well as the publication of the PARTNER 3 low-risk trial showing TAVI to be noninferior to surgery at 2 years.
No Significant Differences
The VIVA study randomized 151 patients with severe aortic stenosis and small aortic annuli(mean age 75 years; 93% women) from 15 hospitals to TAVI or SAVR.
Final inclusion of patients in the trial was based on a mean aortic annular diameter < 23 mm and a minimal diameter ≤ 21.5 mm as evaluated by contrast CT. For the overall cohort, the mean and minimal aortic annular diameters on CT were of 21.1 mm and 18.8 mm, respectively. More than 80% of patients in both groups had hypertension and about one-third had diabetes.
Valve systems used for TAVI were the balloon-expandable SAPIEN 3/ULTRA valve (Edwards Lifesciences), the self-expandable Evolut R/PRO/PRO+ valve (Medtronic), and the Acurate neo/neo2 valve (Boston Scientific). In surgical patients, any approved valve could be used, and aortic root enlargement decisions were left to the discretion of the surgeon. It was used in just 7% of cases.
At 30 days, there were no differences between treatment groups in rates of mortality or stroke. However, major or life-threatening bleeding occurred in 7.8% of TAVI patients and 21.6% of SAVR patients (P = 0.021), while new-onset atrial fibrillation (AF) occurred in 6.5% and 27.0%, respectively (P ≤ 0.001).
For the primary outcomes of severe PPM or moderate-severe AR at 60 days, there was no AR in either group, while PPM occurred in 5.6% of the TAVI group and 10.3% in the SAVR group (P = 0.298).
At median follow-up of 2 years, the rate of death was 9.1% in the TAVI group and 8.1% in the SAVR group, while stroke occurred in 3.9% and 4.1%, respectively, and cardiac hospitalization in 19.5% and 20.3%, respectively (P = 1.0 for all). The most common cause of death was cardiac (53.8%), and the most common reason for cardiac rehospitalization was heart failure events (33%).
At 2 years, the rate of new-onset AF remained significantly higher in the surgery than TAVI groups (31% vs 10%; P = 0.004).
Echocardiographic evaluation was performed at 60 days after the procedure, a departure from the predischarge echocardiograms that many studies include. The VIVA investigators say the delay was intended to avoid “suboptimal quality due to limited acoustic window post-SAVR,” as well as “hyperdynamic conditions (secondary to periprocedural inflammation, anemia, or arrhythmias).”
Lessons for the Future
The authors note that the 2-year mortality rate of 8-9% in VIVA is higher than that seen in PARTNER 3 and Evolut Low Risk, both of which reported mortality rates under 5%. Slightly higher surgical risk and older age in the VIVA participants may account for this finding, they add, as may factors specific to women, who accounted for the majority of the study population.
In addition to being stopped before planned enrollment was completed, the study did not have CT core lab adjudication, although it did have echocardiographic core lab. To TCTMD, Rodés-Cabau said while it is a limitation, budget was primary reason it was not available, with the investigator-initiated trial intended to be as pragmatic as possible.
“The advantage of the trial is that it reflects exactly real-world practice,” he said. “Maybe we were putting a bit of pressure on the surgeons, on the teams, to perform well, to implant valves that they [thought] could work well in these patients, but in any case, it was really a mix of different valves as we see in real-world practice.”
Cardiac surgeons in the trial had access to a preprocedural cardiac CT, with accurate measurements of the aortic annulus in all patients, another factor that Rodés-Cabau and colleagues says may have positively influenced the surgical strategy.
One thing that is considerably different from practice in the United States, noted discussant Tsuyoshi Kaneko, MD (Washington University School of Medicine in St. Louis, MO), following the presentation, is that approximately 60% of patients in VIVA were implanted with self-expandable valves, raising some question about the generalizability of the results.
Speaking with TCTMD, Kaneko said ongoing studies, like the SMART trial, will add more needed evidence to contextualize discussions around treatment and outcomes in patients with small aortic annuli. One unusual finding of VIVA is that there was just a single case of valve migration that required conversion to surgery among the 156 patients.
“I would think that the valve migration would occur more frequently with larger valves, and I do think that it is the issue of sizing [and] the technique. So I don't know if it's particularly relevant to this small annulus group,” Kaneko said. “I’m not too worried about it. I would be more concerned if this was a large valve study. We used to see a lot of migrations when this technology was first introduced. A lot of it was lack of experience, lack of standardized measurement methods, but that has changed over time.”
“These are really important data,” concluded moderator Robert Bonow, MD (Northwestern University Feinberg School of Medicine, Chicago, IL), who added that he will take the results of the VIVA trial into consideration when speaking with patients, especially older female patients with small aortic annuli, about their treatment options.
L.A. McKeown is a Senior Medical Journalist for TCTMD, the Section Editor of CV Team Forum, and Senior Medical…
Read Full BioSources
Rodés-Cabau J, Ribeiro H, Mohammadi S, et al. Transcatheter or surgical aortic valve replacement in patients with severe aortic stenosis and small aortic annulus: a randomized clinical trial. Circulation. 2023;Epub ahead of print.
Disclosures
- The study was partially funded by an unrestricted research grant from Boston Scientific.
- Rodés-Cabau reports institutional research grants from and consulting for Edwards Lifesciences and Medtronic.




Comments