Zero CAC? LDL Cholesterol May Not Predict MI, ASCVD
Patients with elevated LDL and coronary calcium faced increased risks of events, but having zero calcium appeared protective.
In middle-aged, symptomatic patients with evidence of atherosclerosis as measured by coronary artery calcium (CAC), levels of LDL cholesterol are strongly associated with 5-year risk of atherosclerotic cardiovascular disease (ASCVD) events, but the same does not hold true for those with zero CAC, according to a large registry data set.
The findings were maintained in participants of the Multi-Ethnic Study of Atherosclerosis (MESA) with follow-up data over 16 years, which researchers say supports the notion of the “power of zero”: namely, that elevated LDL cholesterol is not something to worry about or treat for those with no CAC.
“If you do not have any atherosclerosis and you are middle-aged, then probably it is not too dangerous to have a little elevated LDL cholesterol,” lead author Martin Bødtker Mortensen, MD, PhD (Aarhus University Hospital, Denmark), told TCTMD. “If [the patient] is in the gray zone of risk, then you might withhold therapy, but of course, if you have a lot of other risk factors, then you might start prevention.”
He noted that he has worked in this field for many years, but said the findings are prompting him, unexpectedly, to rethink his practice. “We knew that adults with zero calcium had low risk,” he said. “But because some of them do develop myocardial infarction, some do develop stroke, [the fact] that LDL cholesterol is not a risk factor for those is surprising. Diabetes is still a risk factor in those who have zero calcium, smoking is still a risk factor for cardiovascular disease in those who have zero calcium, but we could not find that LDL cholesterol was a risk factor for these events.”
Similarly, Matthew Budoff, MD (Harbor UCLA Medical Center, Torrance, CA), who commented on the study for TCTMD, said the findings strongly reinforce what he had previously believed. “Historically, we have said that LDL cholesterol is a great target of therapy but not a great predictor of who is going to develop events,” he said. “And if you look overall in the population, [someone with] an LDL of 130 is as likely to never have an event as to have an event. But this is very interesting, suggesting that once you have atherosclerosis, LDL becomes a pretty robust predictor.”
This is likely tied to why statins work “so dramatically” to reduce cardiovascular events in patients with CAC, Budoff added.
LDL Cholesterol and CAC
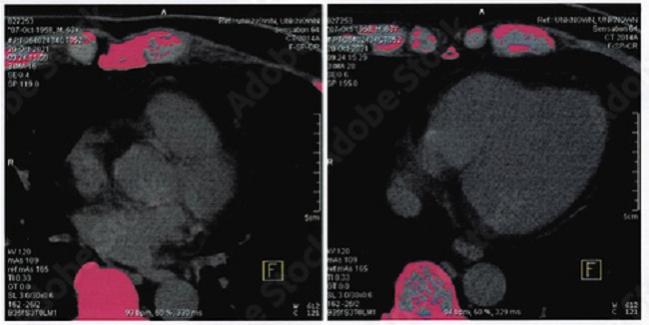
For the study, published online last week in Circulation, Mortensen and colleagues included 23,132 consecutive symptomatic patients (mean age 57 years; 55% women) who underwent coronary CT angiography (CTA) to assess for CAD as part of the Western Denmark Heart Registry between 2008 and 2017. The 53% of patients with no evidence of CAC were on average younger than those with calcium (53 vs 62 years).
Over a median follow-up period of 4.3 years, the rates of first MI and ASCVD event within the total cohort were 1.2% and 2.4%, respectively, but both events were more than doubled in patients with CAC levels greater than zero.
As expected, LDL cholesterol tracked with risk: for every 38.7 mg/dL increase, investigators saw an increased risk of ASCVD events (adjusted HR 1.14; 95% CI 1.04-1.24) and MI (adjusted HR 1.28; 95% CI 1.13-1.44). However, increasing LDL cholesterol was linked to a significantly higher risk of ASCVD events and MI only in those patients with evidence of CAC (adjusted HR 1.18; 95% CI 1.06-1.31 and 1.30; 95% CI, 1.14–1.49, respectively), with no such relationships for those without CAC.
Similarly, while very high LDL cholesterol levels (> 193 mg/dL) were associated with ASCVD events and MI in patients with CAC, this was not seen in those with zero calcium scores.
Notably, diabetes, current smoking, and low HDL cholesterol levels were associated with future ASCVD event risk in patients with zero calcium.
If you do not have any atherosclerosis and you are middle-aged, then probably it is not too dangerous to have a little elevated LDL cholesterol. Martin Bødtker Mortensen
Sensitivity analyses of patients with and without CTA-defined atherosclerosis, as well as those excluding patients taking statins at baseline, confirmed the primary results. The researchers additionally validated their findings using 16 years of data from MESA.
Mortensen stressed that these data are limited to middle-aged patients and only to events over 5 years, not longer. “If you look at 15 or 16 years of follow-up, then some of these individuals will have developed atherosclerosis and then LDL might be associated with cardiovascular disease,” he said. “But we can say now pretty certainly that, at least in the next 5 to 10 years, elevated LDL cholesterol is not a strong risk factor for cardiovascular disease events in those who have zero coronary artery disease or zero atherosclerosis in middle age.”
He said he hopes to follow the patients in this study even further. “That would be one of the most important things to do: to see, okay, is this result robust when we also look at 20 or 25 years?”
For the time being, he added, while the MESA findings “support that these results extend beyond the 5- to 10-year follow-up we have in our study, still, you should really be careful not to extrapolate these results to young individuals, to individuals who have genetically raised cholesterol, like in familial hypercholesterolemia, and you should not extrapolate these results to 20 or 25 years of follow-up,” he advised.
No CAC, No Statins
For Budoff, the study “reinforces strongly that if patients do not have coronary calcium that putting them on a statin is likely to be futile.”
However, for patients with CAC, “statins become quite important because LDL becomes a robust predictor of future events,” Budoff continued. “I think it reinforces what we call the ‘power of zero,’ and that is in our current cholesterol guidelines. . . . However, if they have plaque, this further reinforces the need for more-aggressive treatment and getting that LDL as low as possible.”
This is very interesting, suggesting that once you have atherosclerosis, LDL becomes a pretty robust predictor. Matthew Budoff
The data don’t “totally answer the longitudinal question of whether the high LDL starts the atherosclerotic process or not,” Budoff said. “We believe that it does because people with familial hyperlipidemia, who are born with high LDLs, tend to develop heart disease at an earlier age. But this reminds us that about half the population is not susceptible to LDL cholesterol.”
Most clinicians in this space have seen the “90-year-old women who have crazy high LDLs who never develop heart disease, but we've never quantified it as well as this does,” Budoff added.
Going forward, prospective data in this space are what’s needed to ultimately answer the question of CAC’s predictive power. The ongoing ROBINSCA trial in Europe will hopefully provide just that, Budoff said.
Yael L. Maxwell is Senior Medical Journalist for TCTMD and Section Editor of TCTMD's Fellows Forum. She served as the inaugural…
Read Full BioSources
Mortensen MB, Dzaye O, Bøtker HE, et al. Low-density lipoprotein cholesterol is predominantly associated with atherosclerotic cardiovascular disease events in patients with evidence of coronary atherosclerosis: the Western Denmark Heart Registry. Circulation. 2023;Epub ahead of print.
Disclosures
- The study was funded by Aarhus University Hospital.
- Mortensen reports receiving lecture fees from Sanofi, Amgen, Amarin, and AstraZeneca.





Comments