Access to Cardiac PET Limited in Many Parts of the US
Growing interest in the technology plus a novel tracer on the way may induce change in coming years, says Marcelo Di Carli.

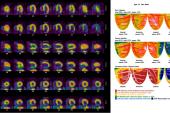
Access to cardiac positron emission tomography (PET) varies widely across the United States, with large swaths of the Midwest having few and in some cases no centers within a reasonable radius that offer the advanced imaging technology, a study suggests.
While areas near large metropolitan cities like New York, Boston, Los Angeles, and Dallas have significant availability and geographic proximity of cardiac PET facilities, four states plus the entire territory of Puerto Rico have none, according to results published in JACC: Cardiovascular Imaging.
“This is a shared responsibility among all of us [as] physicians, regulators, professional societies, and payers to make this modality available for our patients where appropriate,” study co-author Mouaz Al-Mallah, MD (Houston Methodist DeBakey Heart and Vascular Center, TX), told TCTMD. “Right now, there is disparity with some patients needing it but not having access to it.”
Al-Mallah and colleague Ahmed Sayed, MBBS (Houston Methodist DeBakey Heart and Vascular Center), used 2021 data from the US Centers for Medicare & Medicaid Services to obtain addresses of providers who billed Medicare for cardiac PET services. They then calculated the number of facilities offering cardiac PET in the United States and the number of those centers per 1,000,000 residents of each state plus the District of Columbia and Puerto Rico, and mapped distances to the centers.
Of 660 facilities offering cardiac PET, the median distance per state was 19.7 km. However, approximately 44.2 million people, or 13.2% of the US population, were estimated to live more than 100 km away from the closest center.
According to Al-Mallah and Sayed’s calculations, patients residing in several states in the Midwest could have to travel 200 to 500 km to get to the nearest center that offers cardiac PET.
“Obviously it's more available in more dense areas of the country and less available in less dense areas, but even in these dense places there are different driving or access times just to get to the modality itself,” Al-Mallah noted.
Hurdles to Access
Growing interest in cardiac PET had led to changes in guidelines, with the most recent 2024 European Society of Cardiology guidelines for the management of chronic coronary syndromes giving it several class Ib and IIa indications, Al-Mallah noted.
“This modality is also the test of choice for obese patients and we're living in an obesity epidemic,” he added. “The Midwest has a very high obesity rate and there are many patients there who may not get access to this modality, [so] the implications for those patients of not getting the most appropriate testing modality could be serious.”
Among all the US states, Texas had the highest number of PET centers at 96, followed by California at 80, and Florida at 78. In the mapped out data included in the study, large clusters of centers offering the technology also can be seen in the New York/New Jersey/Connecticut area and up through Massachusetts. However, Montana, Rhode Island, West Virginia, and Wyoming, in addition to Puerto Rico, had none.
This is a shared responsibility among all of us [as] physicians, regulators, professional societies, and payers to make [PET] available for our patients where appropriate. Mouaz Al-Mallah
Marcelo Di Carli, MD (Brigham and Women's Hospital, Boston, MA), who was not involved in the study, said while he didn’t find the data surprising, they are more of a reflection on how the technology is being used than on where PET centers are located. He added that if the search was for CPT codes for oncologic PET imaging, the map would look quite different and include many more centers throughout the US, with the number of PET installations estimated to be around 2,000. In other words, while the physical scanners may be present, they may be limited to things like oncologic use.
“The biggest hurdle to cardiac use has been access to the radiopharmaceutical,” Di Carli said. For hospitals or free-standing facilities with PET scanners to be willing to enter into contracts to purchase rubidium-82, for example, they have to justify the need for it.
“I think many facilities may not have the confidence that they will have the patient population to offset that, and they may be reluctant,” he noted.
A Different Future Ahead
But all that may be about to change with hopes running high that flurpiridaz F-18 will be approved soon, Di Carli added. Last year, the second of two positive phase III trials was published, showing that the novel tracer outperformed invasive coronary angiography for the diagnosis of CAD. It also was significantly better than technetium-99m-labeled single-photon emission computed tomography (SPECT) in CAD detection overall and in subgroups including those with obesity and in women.
According to Di Carli, the approval of flurpiridaz F-18 will remove a major barrier to cardiac PET by allowing for ordering of individual unit doses through pharmacies rather than investing in contracts for a large supply from third parties.
“It will be interesting to see what happens with access once it becomes available,” he said. “We know that PET is simply a much better test than [SPECT] because it provides you with more accurate information. We call the quantitative PET the functional coronary angiogram because you can get a lot of the information that interventionalists have shown us that you can get in the cath lab . . . and now with PET you can do it noninvasively at a very low radiation dose to patients.”
The horse is out of the barn and now physicians recognize the incremental value of [cardiac PET] in so many different areas of cardiology. Marcelo Di Carli
A separate paper published by Al-Mallah’s group last month in the Journal of Nuclear Cardiology gives insight into trends in cardiac imaging, showing a relative reduction in the use of cardiac SPECT in the last few years and fast growth in cardiac PET. In fact, cardiac PET is now the second most frequently used modality for CAD assessment in the Medicare population, the study shows.
“So, the horse is out of the barn and now physicians recognize the incremental value of [cardiac PET] in so many different areas of cardiology,” Di Carli added.
Both Al-Mallah and Di Carli said they would hope that 10 years from now access to PET across the US will look much different from its current limited scope.
L.A. McKeown is a Senior Medical Journalist for TCTMD, the Section Editor of CV Team Forum, and Senior Medical…
Read Full BioSources
Sayed A, Al-Mallah M. Geographic proximity to cardiac positron emission tomography facilities across the United States. J Am Coll Cardiol Img. 2024;Epub ahead of print.
Disclosures
- Sayed reports no relevant conflicts of interest.
- Al-Mallah reports research support from Siemens unrelated to the work; and is also a consultant to General Electric and Jubilant.
- Di Carli is the editor-in-chief of the Journal of Nuclear Cardiology.




Comments