PET-Guided Strategy Lowers Risk, Boosts Outcomes in Stable CAD: CENTURY
Comprehensive lifestyle and medical therapy interventions, guided by serial imaging, can impact risk in stable patients.
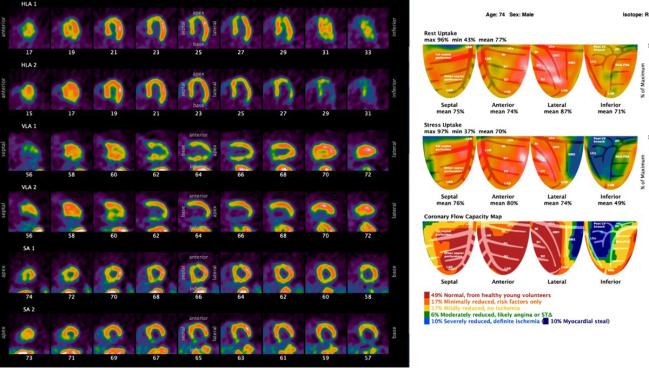
Photo Credit: Nils P. Johnson
Using serial PET imaging to guide revascularization decisions, alongside a comprehensive strategy of risk-factor control and lifestyle changes, significantly reduces coronary artery disease risk and improves adherence to healthy habits over 5 years of follow-up, according to results from the CENTURY randomized trial.
Presented today at the 2023 American Society of Nuclear Cardiology (ASNC) annual meeting, CENTURY suggests this integrated approach, when compared with standard practice, can decrease major adverse cardiovascular events—the study’s secondary endpoints—while reducing the number of patients sent for revascularization.
Nils Johnson, MD, PhD (McGovern Medical School at UTHealth/Memorial Hermann Hospital-Texas Medical Center, Houston), who presented the data at ASNC, believes their intensive, PET-guided intervention can be replicated in real-world practice.
CENTURY, launched in 2008, was ahead of its time in that “we were much more aggressive about lipid management,” he told TCTMD. “I think what we were doing back then has really been backed up by the evolution we've seen with more aggressive lipid management with the newer agents as well. More aggressive diabetes control was also a big part of it, both through dieticians counseling patients and then trying to get the hemoglobin A1C tuned up. That mirrors some of the new drugs that have come along for diabetes within the last little period.”
The goal of the CENTURY trial was to determine if an imaging-guided strategy that included intensive lifestyle changes and optimal medical management to reach specific risk-factor targets could reduce patient risk and improve clinical outcomes. In the intervention arm, quantitative PET myocardial perfusion imaging was performed at baseline, 2, and 5 years, with scans reviewed to guide interventional decisions. These patients also had regular access to nurses, nutritionists, and management staff every few months to help them stay on track with medical therapy and a healthy lifestyle.
In the standard treatment arm, patients also underwent PET imaging, had a brief preventive review at baseline, and all treatments were managed by the primary-care physician. Both physicians and patients blinded to PET scan results unless there was a need for immediate PCI or CABG surgery.
In the end, the study included 1,028 high-risk patients with subclinical, suspected, or established CAD randomized to the two treatment strategies between 2009 and 2017. Of those randomized, 42% had a history of CAD, including 26.7% with prior PCI, 9.7% with prior CABG, and 16.1% with prior MI.
“We ended up with a patient population that’s representative of a lot of our clinics,” said Johnson.
Shifting Patient Risk Downward
The primary endpoint of CENTURY was the change in the summed risk score, comprised of 10 modifiable risk factors, including adherence to a healthy diet, and six nonmodifiable risk factors. At 5 years, the final risk scores were 15.4 in the comprehensive group and 16.7 in the standard-treatment group, with changes from baseline of -1.1 and 0.33, respectively (P < 0.0001).
“The comprehensive patients shifted downwards—that is, their risk scores decreased, they became healthier over time—whereas the standard group went the other way,” said Johnson.
The risk of MACE was significantly lower at 5 years in the PET-guided comprehensive-strategy arm (20.5% vs 29.9%; P = 0.0006), as were individual risks of death, death/MI, and coronary revascularization. Of note, the revascularization rate was higher in the standard-care arm (9.6% vs 14.8%; P = 0.01).
Johnson said that while 5 years of follow-up is “above average” for a cardiovascular trial, investigators are planning to track patients for more than a decade. An early snapshot of those longer-term data suggests the comprehensive strategy continues to be associated with less mortality than standard treatment.
As part of the trial, researchers quantified coronary flow capacity by rest-stress PET perfusion imaging, which is a way to assess the physiologic severity of CAD. When patients didn’t have severely reduced coronary flow capacity on PET, the revascularization rate was extremely low (0.4%), said Johnson, emphasizing that such patients are appropriate candidates for medical therapy. Even when coronary flow capacity was severely reduced, revascularization was infrequently performed (10.4%).
“It highlights that having a low coronary flow capacity is a necessary, but not sufficient, criteria for invasive management,” said Johnson. “There are other factors that go along with that, such as the size of perfusion defect, patient symptoms, and other clinical parameters we bring together to make those decisions.”
The National Institutes of Health-funded ISCHEMIA trial, published in 2020, found an invasive strategy with revascularization was no better than conservative management in patients with moderate-to-severe ischemia on stress testing—this led some to question the role of nuclear imaging in patients with chronic CAD. Subsequent analyses also showed that the severity of ischemia did not predict the risk of death or MI over 4 years of follow-up, nor was there a benefit of revascularization in patients with more extensive ischemia.
Johnson pointed out that one-third of patients in CENTURY had a stress-perfusion defect on PET imaging, something that would have triggered a referral for coronary angiography in most clinical practices. With the coronary flow capacity metric, they were able to significantly reduce the number of patients sent to the cath lab for revascularization, suggesting that the “addition of coronary flow layered on top of relative-uptake mapping” can serve as an up-front “gatekeeper” to appropriately select patients for invasive therapy, he said.
Mouaz Al-Mallah, MD (Houston Methodist, TX), president of the ASNC, said coronary flow capacity is not unlike coronary flow reserve (CFR) assessed in the cath lab, but that it takes not only CFR but the amount of stress or hyperemic myocardial blood flow. The CENTURY trial, he told TCTMD, shows that this imaging-based strategy with cardiac PET can have a large impact on not only management decisions, but also clinical outcomes.
“What we see here is that it not only is de-risking them, which is a mathematical exercise, but this is potentially saving lives,” he said.
In terms of what’s driving the reduction in clinical outcomes, researchers can’t say for sure. For example, the magnitude of change in LDL cholesterol or blood pressure can’t explain the reduction in MACE, nor can the judicious deployment of coronary revascularization. Johnson suspects “it is a little bit of benefit from a lot of different aspects” of the comprehensive management plan.
CENTURY, he added, was also one of the largest dietary intervention studies done to date, noting that researchers want to look more closely at these data to determine what aspects may have impacted outcomes.
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Johnson N, on behalf of the CENTURY investigators. The CENTURY trial: PET-guided RCT of CAD management. Presented at: ASNC 2023. September 29, 2023. Toronto, Canada.
Disclosures
- Johnson reports grant support paid to his institution from Neovasc and CoreAalst. He reports licensing of intellectual property from OpSens Medical paid to his institution.




Comments