COVID-19: TCTMD’s Dispatch for November Week 3
We’re curating a list of COVID-19 research and other useful content, and updating it regularly.

Since March 2020, TCTMD reporter Todd Neale has been writing up breaking news and peer-reviewed research related to COVID-19 every weekday. In July 2021, we transitioned to Mondays, Wednesdays, and Fridays. If you have something to share, tell us. All of our COVID-19 coverage can be found on our COVID-19 Hub.
November 19, 2021
As expected, the US Food and Drug Administration (FDA) on Friday expanded eligibility for booster doses of the COVID-19 vaccines from Moderna and Pfizer/BioNTech to include all adults who have completed primary vaccination with any FDA-authorized or -approved vaccine (which also includes the Janssen vaccine from Johnson & Johnson). The boosters can be administered at least 6 months after completion of the series with one of the mRNA vaccines and at least 2 months after the single-shot Janssen vaccine. The Advisory Committee on Immunization Practices (ACIP), which provides guidance to the US Centers for Disease Control and Prevention (CDC), voted to broaden eligibility after the FDA’s announcement (STAT).
 As winter approaches, a surge in COVID-19 cases is causing many countries in Europe to start locking down again, Reuters reports. Austria has gone the furthest, expanding what had been a lockdown for unvaccinated residents to include all people, starting Monday; Germany has warned that it might do the same. Austria has additionally said that all of its citizens will be required to get vaccinated starting February 1. The country has one of the lowest vaccination rates in western Europe.
As winter approaches, a surge in COVID-19 cases is causing many countries in Europe to start locking down again, Reuters reports. Austria has gone the furthest, expanding what had been a lockdown for unvaccinated residents to include all people, starting Monday; Germany has warned that it might do the same. Austria has additionally said that all of its citizens will be required to get vaccinated starting February 1. The country has one of the lowest vaccination rates in western Europe.
The European Medicines Agency (EMA) has released guidance on the use of molnupiravir, the oral COVID-19 pill from Merck and Ridgeback Biotherapeutics, saying that it can be used for adults with COVID-19 who do not require supplemental oxygen and who are at increased risk of developing severe disease. The pill is not yet authorized for use, and the “EMA issued this advice to support national authorities who may decide on possible early use of the medicine prior to marketing authorization, for example in emergency use settings, in light of rising rates of infection and deaths due to COVID-19 across the EU.” The EMA also has started a review of ritonavir, the oral pill from Pfizer shown to reduce hospitalization and death among nonhospitalized patients with mild-to-moderate COVID-19 at high risk for progression.
The European Society of Cardiology (ESC) has issued new, two-part guidance on managing cardiovascular disease during the COVID-19 pandemic, published in the European Heart Journal. “Acknowledging the rapidly changing field, the ESC task force hopes the documents—one addressing ‘epidemiology, pathophysiology, and diagnosis’ and the other covering ‘care pathways, treatment, and follow-up’—can help tired physicians manage the various manifestations of cardiovascular disease associated with the virus,” TCTMD’s Yael Maxwell reports.
New data on AstraZeneca’s antibody cocktail—called AZD7442 or Evusheld—shows that it provides strong protection through at least 6 months, according to a company press release. For preventing the development of symptomatic COVID-19 in high-risk or immunocompromised people, it had an 83% reduced risk relative to placebo at 6 months. And in outpatients with COVID-19, it reduced the risk of severe COVID-19 or death by 88%. Reuters has more.
 A scientist who examined information on the earliest SARS-CoV-2 cases in Wuhan, China, has suggested that the first known patient was a vendor in the large Huanan Market, at which live mammals susceptible to infection with coronaviruses were sold, calling into question the conclusions of an earlier World Health Organization (WHO) investigation. His review, published in Science, “will revive, though certainly not settle, the debate over whether the pandemic started with a spillover from wildlife sold at the market, a leak from a Wuhan virology lab, or some other way,” a New York Times story notes.
A scientist who examined information on the earliest SARS-CoV-2 cases in Wuhan, China, has suggested that the first known patient was a vendor in the large Huanan Market, at which live mammals susceptible to infection with coronaviruses were sold, calling into question the conclusions of an earlier World Health Organization (WHO) investigation. His review, published in Science, “will revive, though certainly not settle, the debate over whether the pandemic started with a spillover from wildlife sold at the market, a leak from a Wuhan virology lab, or some other way,” a New York Times story notes.
A study in Morbidity and Mortality Weekly Report highlights the risk of remaining unvaccinated, showing that SARS-CoV-2 infection was three times more likely, hospitalization was twice as likely, and death was seven times more likely among unvaccinated versus vaccinated people living in Oregon and Washington during widespread circulation of the Delta variant.
Another MMWR report provides estimates of the impact of hospital strain during the pandemic on excess deaths: “If intensive care unit (ICU) bed use nationwide reached 75% capacity, an estimated 12,000 additional excess deaths would occur nationally over the next 2 weeks. As hospitals exceed 100% ICU bed capacity, 80,000 excess deaths would be expected in the following 2 weeks.” That indicates, the authors say, “the importance of controlling case growth and subsequent hospitalizations before severe strain.”
The aspirin results from the RECOVERY trial, released in top-line form back in June, have been published in the Lancet. When added to usual care, aspirin did not reduce the risk of dying in the first 28 days, although it did slightly shorten the duration of hospitalization (from a median of 9 to 8 days). Aspirin use was associated with a lower rate of thrombotic events (4.6% vs 5.3%) but also a higher rate of major bleeding (1.6% vs 1.0%). “Not the result we hoped for, but important to know nonetheless,” one of the trial investigators said on Twitter.
 Loss of smell is an “emerging public health concern” during the COVID-19 pandemic, according to a study in JAMA Otolaryngology – Head & Neck Surgery. “This analysis of new daily cases of COVID-19, acute incidence of olfactory dysfunction, and rates of recovery suggest that more than 700,000, and possibly as many as 1.6 million, US individuals experience chronic olfactory dysfunction because of SARS-CoV-2,” the authors say.
Loss of smell is an “emerging public health concern” during the COVID-19 pandemic, according to a study in JAMA Otolaryngology – Head & Neck Surgery. “This analysis of new daily cases of COVID-19, acute incidence of olfactory dysfunction, and rates of recovery suggest that more than 700,000, and possibly as many as 1.6 million, US individuals experience chronic olfactory dysfunction because of SARS-CoV-2,” the authors say.
November 17, 2021
The number of weekly COVID-19 cases ticked up 6% compared with the previous week, driven by increases in the Americas and the European and Western Pacific regions, according to the latest update from the World Health Organization (WHO). Only Europe saw an increase in new deaths (by 5%), however. The Associated Press provides more details.
 NPR delves into the concerning rise in US COVID-19 cases as Americans make plans for the upcoming holiday season. After cases fell from the middle of September to late October, the country is now averaging more than 83,000 cases per day, a 14% increase compared with the prior week. “Growing outbreaks in the Midwest and Northeast are most responsible for pushing up the national numbers, and that comes after many weeks of high case counts and stress on states in the Mountain West where some hospitals are dealing with crisis levels of patients.” The AP details new surges in Michigan and Minnesota.
NPR delves into the concerning rise in US COVID-19 cases as Americans make plans for the upcoming holiday season. After cases fell from the middle of September to late October, the country is now averaging more than 83,000 cases per day, a 14% increase compared with the prior week. “Growing outbreaks in the Midwest and Northeast are most responsible for pushing up the national numbers, and that comes after many weeks of high case counts and stress on states in the Mountain West where some hospitals are dealing with crisis levels of patients.” The AP details new surges in Michigan and Minnesota.
Pfizer has asked the US Food and Drug Administration (FDA) to authorize its antiviral pill—ritonavir, which will be marketed under the name Paxlovid—to treat unvaccinated patients with COVID-19 who have a high risk of becoming severely ill, the New York Times reports. The treatment was shown in a phase II/III trial to reduce the risk of COVID-19-related hospitalization or death from any cause. The Biden administration reportedly plans on building a stockpile of the pill, with enough for about 10 million courses of treatment to be used over the next 10 months. One Tuesday, Pfizer announced a licensing agreement—similar to one signed by Merck for its antiviral pill, molnupiravir—that would expand production of the drug for low- and middle-income countries.
Two trials presented recently at the virtual American Heart Association (AHA) 2021 Scientific Sessions scratch two therapies off the list of treatments for COVID-19: one using icosapent ethyl (Vascepa; Amarin) in outpatients (PREPARE-IT 2) and the other testing P2Y12 inhibitors in patients who are hospitalized but not critically ill (ACTIV-4a). Both trials failed to show a clinical benefit in the target patient populations. “To know that something does not work, in my opinion, is just as helpful as knowing that it does work, because then we move on,” Amit Khera, MD, told TCTMD.
The European Medicines Agency (EMA) said Wednesday that it has begun evaluating an application for authorization of Novavax’s COVID-19 vaccine. The assessment will be done on an accelerated schedule, with a decision possible within weeks if the submitted data are adequate, said the agency, which had already been looking at some of the data during a rolling review. The vaccine, Novavax noted in a press release, is being studied in two phase III trials: “a trial in the UK that demonstrated efficacy of 96.4% against the original virus strain, 86.3% against the Alpha (B.1.1.7) variant, and 89.7% efficacy overall; and the PREVENT-19 trial in the US and Mexico that demonstrated 100% protection against moderate and severe disease and 90.4% efficacy overall. It was generally well tolerated and elicited a robust antibody response.”
 Use of an automated remote monitoring service involving regular text message check-ins—called COVID Watch—was associated with a lower risk of dying among outpatients with COVID-19, according to a study in the Annals of Internal Medicine. Patients participating in the program had more telemedicine encounters, ED visits, and hospitalizations, and presented to the ED sooner, compared with nonparticipants. “Our evaluation found that a small team of five or six nurses staffing the program during some of the most hectic days of the pandemic directly saved a life every 3 to 4 days,” one of the researchers said in a press release.
Use of an automated remote monitoring service involving regular text message check-ins—called COVID Watch—was associated with a lower risk of dying among outpatients with COVID-19, according to a study in the Annals of Internal Medicine. Patients participating in the program had more telemedicine encounters, ED visits, and hospitalizations, and presented to the ED sooner, compared with nonparticipants. “Our evaluation found that a small team of five or six nurses staffing the program during some of the most hectic days of the pandemic directly saved a life every 3 to 4 days,” one of the researchers said in a press release.
Telehealth played an important role in keeping Medicare beneficiaries connected to their doctors, a study in the Journal of Evaluation in Clinical Practice confirms. More than half of primary care doctors (58%) provided telehealth services, compared with only 26% to 28% of specialists. Less than 8% of beneficiaries said they were unable to receive care because of COVID-19. Changes to Medicare policies, the authors say, “likely increased the proliferation and utilization of telehealth services during the COVID-19 pandemic, providing important access to care for certain populations.”
The Infectious Diseases Society of America (IDSA) has released new guidelines on infection protection for healthcare workers caring for patients with suspected or known COVID-19, published in Clinical Infectious Diseases. “These recommendations should serve as a minimum for personal protective equipment use in healthcare facilities and do not preclude decisions based on local risk assessments or requirements of local health jurisdictions or other regulatory bodies,” the authors note.
Use of selective serotonin reuptake inhibitors (SSRIs), particularly fluoxetine or fluvoxamine, is associated with a lower risk of mortality among patients with COVID-19, researchers report in JAMA Network Open. “These findings suggest that SSRIs, if proven effective, could be a therapeutic option to reduce mortality among patients with COVID-19,” the authors say, acknowledging the need for additional studies.
 Two other papers in the same journal provide insights into the mental health toll of the pandemic. One conducted in the UK shows that SARS-CoV-2 infection is associated with greater risks of fatigue and sleep problems, and the other reveals that inpatient stays for eating disorders in the US rose during the pandemic.
Two other papers in the same journal provide insights into the mental health toll of the pandemic. One conducted in the UK shows that SARS-CoV-2 infection is associated with greater risks of fatigue and sleep problems, and the other reveals that inpatient stays for eating disorders in the US rose during the pandemic.
November 15, 2021
Austria, facing a 7-day infection rate exceeding 800 cases per 100,000 people, has issued a lockdown for about 2 million people who haven’t gotten their COVID-19 shots. The unvaccinated—which make up about 35% of the country’s population—will be allowed to leave home only for necessities like working or buying food, the BBC reports, quoting Chancellor Alexander Schallenberg: “We are not taking this step lightly, but unfortunately it is necessary.”
As noted in Newsweek, the European Medicines Agency (EMA) is investigating six reported cases of capillary leak syndrome among patients who received Moderna’s Spikevax vaccine, out of 61.6 million disease administered in Europe since its authorization in January 2021. As of now, there’s no evidence of a causal link, the EMA says.
Just last week, Pfizer and BioNTech announced they’re seeking an amendment to the US Food and Drug Administration (FDA) emergency use authorization that expands the booster dose to include all people ages 18 and older. The request is based on results the companies released back in October showing a third shot gives 95.6% efficacy against COVID-19.
Jousting over COVID-19 vaccine mandates continues around the United States, however. “The Oklahoma National Guard has rejected the Defense Department’s requirement for all service members to receive the coronavirus vaccine and will allow personnel to sidestep the policy with no repercussions, an order from the governor that could serve as a blueprint for other Republican-led states that have challenged Biden administration mandates,” says the Washington Post.
 In New York, dozens of city sanitation workers have been suspended without pay while authorities investigate whether they were using fake vaccine cards, the New York Times reports.
In New York, dozens of city sanitation workers have been suspended without pay while authorities investigate whether they were using fake vaccine cards, the New York Times reports.
In the state of Texas, Houston Methodist Hospital has suspended privileges for a doctor who used her personal Twitter account to praise ivermectin and criticize vaccine mandates. Business Insider has the story.
These opinions, which are harmful to the community, do not reflect reliable medical evidence or the values of Houston Methodist, where we have treated more than 25,000 COVID-19 inpatients, and where all our employees and physicians are vaccinated to protect our patients. (2/5)
— Houston Methodist (@MethodistHosp) November 12, 2021
Meanwhile, the US is also confronting the reality that their recent drop in cases may not last, according to the Wall Street Journal, which reports COVID-19 is on the rise in the upper Midwest, Southwest, and some areas of the Northeast. “While the Southeast cools off from its summer surge, other regions are under pressure, including places where colder weather has brought people back indoors where the virus can more easily spread,” the article notes.
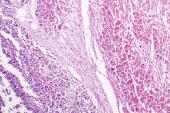
Given that COVID-19 mortality is higher in men than in women, a paper published in JAMA Network Open explored the possibility that androgen deprivation therapy (ADT) might be protective for male patients with prostate cancer. Unfortunately, the cohort study found no such relationship: 30-day mortality rates were 15% and 14%, respectively, with and without ADT. “However, large ongoing clinical trials will provide further evidence on the role of ADT or other androgen-targeted therapies in reducing COVID-19 infection severity,” Andrew L. Schmidt, MD (Dana-Farber Cancer Institute, Boston, MA), and colleagues write.
Also in JAMA Network Open, another investigation looks at work-family conflict and mental health among 276 physician parents during the pandemic. Overall, there was an increase in gender inequality within medicine, researchers conclude. “Mothers were more likely than fathers to be responsible for childcare or schooling and household tasks, to work primarily from home, to reduce their work hours, and to experience work-to-family conflict, family-to-work conflict, and depressive and anxiety symptoms.”
 At the Lincoln Children’s Zoo, in Nebraska, three snow leopards have died of COVID-19 complications about 1 month after testing positive, the New York Times reports. The animals, along with COVID-positive Sumatran tigers living in the same facility, had been given steroids and antibiotics, but the zoo didn’t say whether they also had been vaccinated. “This loss is truly heartbreaking, and we are all grieving together,” their statement said.
At the Lincoln Children’s Zoo, in Nebraska, three snow leopards have died of COVID-19 complications about 1 month after testing positive, the New York Times reports. The animals, along with COVID-positive Sumatran tigers living in the same facility, had been given steroids and antibiotics, but the zoo didn’t say whether they also had been vaccinated. “This loss is truly heartbreaking, and we are all grieving together,” their statement said.
TCTMD News Editor Caitlin E. Cox contributed today’s Dispatch.
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full Bio



Comments