Editor’s Pick: TCTMD’s Best Long Reads of 2024
Touchy topics, timely analysis, tips for tackling entrenched problems: enjoy some of TCTMD’s best features this year.

We try to be timely at TCTMD. Late-breaking clinical trials at a meeting? We know you want to see results as soon as possible. FDA approvals and recalls? You wanted to hear about those yesterday.
Then, when it comes to interesting and important papers appearing in the medical press, our aim is to provide some context and conversation around these topics, ideally at the same time the articles are being published. After all, there are dozens of different ways to keep abreast of cardiology news online, and timeliness is one way we aim to distinguish ourselves from the pack.
Some stories, though, take time to rise and even longer to bake. These may be related to trends we are noticing in cardiology research and care. They may stem from breaking news stories and our aim, here, is to look deeper and wider, to anticipate what the ripple effects will be. As 2024 winds to close, I’ve looked back and selected a handful of feature stories that took days or weeks—even months—to pull together. All of these, I believe, deserve a little bit of that most precious thing: your time.
Going Solo: Can TAVI Be Performed Without a Surgical Safety Net?
By Michael O’Riordan
Over the last two decades, TAVI procedures have become safer and more standardized, leading some physicians to question the need for on-site surgical backup. On-site surgery is specified in clinical guidelines and expert consensus statements as a prerequisite for TAVI programs. Allowing TAVI programs to open in places with protocols in place for surgical transfer—but no surgeons on the premises—would go a long way to improving access for a procedure that many patients are having trouble getting referrals for. As TCTMD’s Michael O’Riordan reported back in January, for some patients with severe aortic stenosis, such stand-alone TAVI centers might represents their only chance at a new valve.
SEE ALSO: Hearing and Learning From Patients Undergoing AVR
Valvular Heart Disease Has a Diversity Problem
By Yael L. Maxwell
While stand-alone centers might help improve access for patients who get referred for a transcatheter valve, but don’t live anywhere near a major hospital with both SAVR and TAVI options on-site, an even bigger problem is the mix of patients overall. As TCTMD’s Yael Maxwell reported in July, there are “inexplicable differences” in the rates of TAVI by US zip code. Some of the disparities relate to the time at which patients seek care, but a huge driver is remains the lack of diversity, by both race/ethnicity and gender, in clinical trials. Indeed, it’s not even clear that the blockbuster results from major TAVI trials even apply to large swaths of the population.
SEE ALSO: Quick Takes: Megan Coylewright on Diversity and Representation in Clinical Trials
GDMT Uptake Remains Dismal in HFrEF: What’s the Right Fix?
By Todd Neale
Heart failure care has celebrated some of the biggest medical advances of the past decade, with countless large, well-powered trials demonstrating irrefutable benefits of new drugs and devices to patients with both reduced and preserved ejection fractions. The gap, however, between positive science and clinical implementation grows wider and wider. As TCTMD’s Todd Neale noted in his November feature story, study after study after study after study has documented that most patients eligible for foundational guideline directed medical therapy are not receiving it. More and more researchers, however, are trying for creative ways to solve this problem.
SEE ALSO: Beyond the Data: Team Care for HF
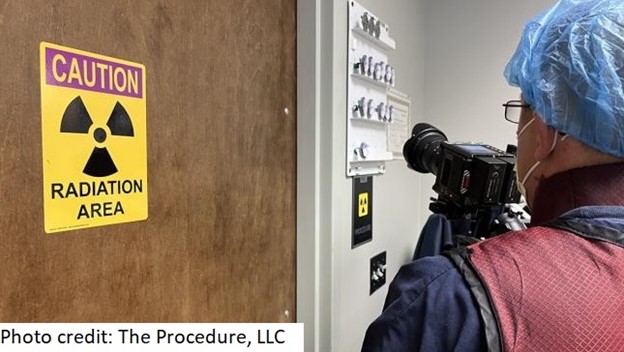
‘Hot’ Doc? Radiation Exposure Risks of Interventionalists Aired in TV Special
By L.A. McKeown
This summer, public broadcasting channels around the United States started airing a documentary entitled Scattered Denial, which tells the stories of physicians whose careers—and in some case, lives—have been shortened by what is for many a ubiquitous occupational hazard: ionizing radiation. As several interventionalists involved in the documentary told TCTMD’s L.A. McKeown, the problem isn’t only due to exposure to the radiation itself, which can cause illness and death, but also the heavy lead required as protection. As one put it, if an automotive factor had these kinds of workplace injuries, it would be shut down. So why is cardiology any different, and what can be done to change the culture?
SEE ALSO: On Record: Radiation in the Cath Lab
Let’s Talk About Sex: How Best to Broach Post-MI Conversations
By Caitlin E. Cox
The World Health Organization considers sexual activity as a health metric, but for many doctors, the topic wasn’t covered in their formal training and few resources exist to help them navigate this tricky subject, even if it is top of mind for patients. While there are a smattering reassuring studies suggesting that there are limited risks and potential benefits to being sexually active after a CVD diagnosis, cardiologists who spoke with TCTMD’s Caitlin E. Cox admitted it’s a topic that both patients and their doctors shy away from. And formal guidance is scant: More than a decade has passed since the American Heart Association released its scientific statement on sexual activity and CVD.
SEE ALSO: Talking Sex: CVD Patients Want to Hear More From Clinicians
Shelley Wood was the Editor-in-Chief of TCTMD and the Editorial Director at the Cardiovascular Research Foundation (CRF) from October 2015…
Read Full Bio





Comments