Embolic Protection During TAVR Reduces Stroke Risk, Single-Center Study Shows
Despite the results and recent FDA approval, embolic protection during TAVR still needs a win for the field to advance, says one expert.
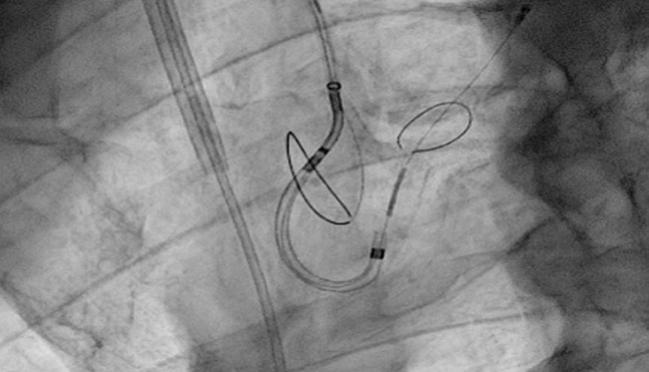
CHICAGO, IL—Use of the Sentinel Cerebral Protection System (Claret Medical), a filter device employed during transcatheter aortic valve replacement procedures, significantly reduces the risk of disabling and nondisabling stroke when compared with no embolic protection in TAVR, a new study shows.
In an analysis of patients treated at a single center, 1.4% of individuals undergoing TAVR with the cerebral protection device had a disabling/nondisabling stroke at 7 days compared with 4.6% of patients who underwent TAVR without the Sentinel device (OR 0.29; P = 0.03).
Presenting the results at TVT 2017, lead investigator Jochen Wöhrle, MD (University of Ulm, Germany), said that when they assessed the same endpoint used in SENTINEL, the clinical trial that helped the device gain approval from the US Food and Drug Administration (FDA), there was a statistically significant reduction in the risk of death, stroke, and acute kidney injury (stage 3) with embolic protection (2.1% vs 7.9% without protection; P = 0.01).
The propensity-matched analysis, which matched patients by STS score, atrial fibrillation, and aortic cusp and left ventricular outflow tract (LVOT) calcification, among other variables, is based on 280 patients treated without protection and 280 treated with the Sentinel device. Wöhrle noted that the device was safe and the technical success rate approached 100%.
To TCTMD, Wöhrle said they have used the device routinely since 2016, absolutely convinced of the benefit of embolic protection based on data from MISTRAL-C and CLEAN-TAVI. While SENTINEL missed its primary endpoint, and from this point of view is a negative trial, he said, there was an observed reduction in the volume of new ischemic lesions on imaging. Moreover, when examining stroke rates in SENTINEL at 72 hours, there was a strong trend toward benefit with embolic protection.
“With our study, we’re not randomized, but we had a larger number of patients and we were able to show a significant reduction in stroke,” said Wöhrle.
Approval Despite Missed Primary Endpoint
Although it’s now available in the United States, and many TAVR experts believe in the intuitive value of embolic protection, the SENTINEL trial missed its primary endpoint. As reported by TCTMD, the 30-day MACCE rates in the cerebral-protection group were noninferior to the performance goal but not statistically different from those of patients treated without the protection device (7.3% vs 9.9%; P = 0.41).
Colin Barker, MD (Houston Methodist, Texas), one of the panel discussants during the TVT session, told TCTMD the German data are interesting and “some of the strongest seen to date,” but he noted that the heart team at his hospital is reluctant to use embolic protection given all the available evidence, specifically the lack of benefit in randomized trials.
“It’s single-center, their experience, and usually that can’t be extrapolated to other centers,” he said. “It’s not that generalizable. It’s compelling enough for them at their institution, but for us we’re not there. We don’t have that kind of data. We may eventually use cerebral embolic protection, but there has to be a randomized trial that shows a true benefit and we don’t have that yet.”
We may eventually use cerebral embolic protection, but there has to be a randomized trial that shows a true benefit and we don’t have that yet. Colin Barker
Barker added, though, that use of embolic protection during SENTINEL and other studies has been shown to be safe and all trends point toward benefit. For this reason, he believes the US approval is appropriate.
“I think there was enough there to have it available, to offer it,” he said. “Obviously, it’s not mandated. If the data were so compelling—that this clearly prevented stroke—I think there would be a stronger influence on us to use it. Basically, it’s available, and it’s up to the hospital and the valve team to decide if this is something they want to use. I think that’s fair.”
Michael Mack, MD (Heart Hospital Baylor, Plano, TX), who also participated in the panel discussion, pointed out that the Sentinel device costs approximately $3,000, which is going to be an issue. While there is a new technology add-on payment now under consideration by the Centers for Medicare & Medicaid Services (CMS), it won’t be available until 2018, according to Mack. If approved, it will cover roughly half the cost of the device.
“If you’re dealing with TAVR, which has close margins right now, and you add $3,000 of costs onto it, and there isn’t a strong evidence base of benefit, it’s hard for clinicians to sell their hospital administrators on why they should add this device,” Mack said. “Those are the realities of the world we all live in right now.”
Most on Board With Embolic Protection, but Not All
During the session, which was devoted to cerebral protection and included discussions on the development of consistent definitions of neurologic injury, as well as experience with another device not yet FDA approved, the TriGuard cerebral protection system (Keystone Heart), most of the physicians agreed that if they were to undergo TAVR, they would opt for cerebral protection, given the amount of debris captured in the device filters during procedures.
Nicholas Van Mieghem, MD (Thoraxcenter, Rotterdam, the Netherlands), said he is “quite convinced cerebral embolization is a proven issue after TAVR and that with filter-based protection [physicians] will capture a lot of the debris.” The results from the German researchers, along with other available data including a positive meta-analysis of SENTINEL, CLEAN-TAVI, and MISTRAL-C that was presented today by Axel Linke, MD (University of Leipzig, Germany), show embolic protection is working, said Van Mieghem.
Despite the positive analysis by the German researchers, as well as the “compelling evidence” from other clinical trials, Jeffrey Moses, MD (Columbia University Medical Center, New York, NY), said the embolic protection field still needs a positive trial. “I think we still need to get on the books,” he said, citing the lack of a “win” for embolic protection in randomized controlled trials. The “tragedy” of SENTINEL is that if it was sufficiently powered—the trial included just 363 patients—“we could have had a clinically relevant trial,” said Moses.
To TCTMD, Wöhrle said that from an “academic” perspective, there is a need for randomized trial showing a benefit for embolic protection. “Of course we need a randomized trial to be absolutely convinced, but putting all the data together—three randomized trials and our analysis, which is the largest worldwide so far—there’s no harm with the device,” he commented. “You can use it, put it in, and there’s a benefit. You see it on MRI and you see it clinically.”
For Barker, the desire to protect the brain from embolization makes sense, but, he said, “a lot of things make sense intuitively and don’t pan out.” With this in mind, Barker advised physicians to be cautiously optimistic as they move forward. “TAVR has become a fairly simple procedure, and you don’t want to make something simple more complex, which [embolic protection devices] could potentially do,” he said.
For Jean-Michel Paradis, MD (Columbia University Medical Center, New York, NY), another physician who participated in the panel discussion, the existing data are compelling, but he expressed some concern over the enthusiasm for embolic protection, specifically whether future devices could be compared to Sentinel in a noninferior trial design.
In fact, Paradis pointed to a meta-analysis published in Stroke last month, reported on by TCTMD, showing that the use of various embolic protection devices, including Sentinel, was not associated with a reduction in the risk of clinically evident stroke or 30-day mortality.
Alexandra Lansky, MD (Yale University School of Medicine, New Haven, CT), said it’s unlikely a clinical trial testing embolic protection would demonstrate a beneficial effect on mortality, saying such a study would require thousands of patients. However, like others, she believes protecting the brain from embolized debris is the right thing to do, adding that all TAVR patients have some degree of brain injury.
“In the past 5 years, I would say we have learned an awful lot about what we’re doing to the brain of our patients as they undergo these procedures,” she said. “What we know from imaging studies is that basically all patients undergoing TAVR have some [central nervous system] infarction. We know this because we can see it on MRI. We know that there are showers of emboli and these are very sizeable.”
Additionally, these infarctions are linked with future clinical symptoms, including cognitive decline, she noted.
Regarding stroke, the rates in the major TAVR trials vary depending how it is defined, ranging from 1.6% to 5.9%. With a broader definition, such as those used by the American Heart Association/American Stroke Association, the risk of mild, moderate, and severe stroke documented by imaging ranges from 15% to 27%, said Lansky.
PHOTO CREDIT: Jochen Wöhrle. Extracted from: A Propensity Score Analysis of Matched TAVR Patients With and Without Cerebral Protection. TVT 2017.
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Presentations at: TVT 2017. June 15, 2017. Chicago, IL.
Disclosures
- Wöhrle reports no conflicts of interest.


Comments