ENBALV: Edoxaban Matches Warfarin After Bioprosthetic Valve Surgery
(UPDATED) Low event rates and short TTRs with warfarin were notable, and questions persist as to which patients truly need OAC.
CHICAGO, IL—Following bioprosthetic valve surgery, anticoagulation with edoxaban (Savaysa; Daiichi Sankyo) is as effective as warfarin, although this strategy might come at a higher cost of bleeding, according to new randomized data. The results were seen, however, on a background of very low time in therapeutic range (TTR) in the warfarin arm, reflecting the difficulty of managing bleeding in the early post-op period.
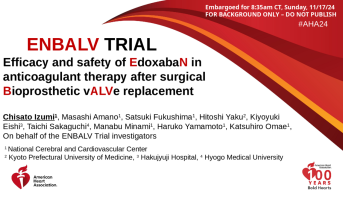
“The ENBALV trial demonstrated that edoxaban is a potential alternative anticoagulant therapy,” said Chisato Izumi, MD, PhD (National Cerebral and Cardiovascular Center, Osaka, Japan), who presented the late-breaking findings today at the American Heart Association 2024 Scientific Sessions. “The availability of edoxaban could offer more flexibility in anticoagulant treatment options after bioprosthetic valve surgery.”
For patients with atrial fibrillation (AF), current US guidelines recommend at least 3 months of anticoagulation following bioprosthetic valve surgery, favoring a vitamin K antagonist given the limited evidence available with non-vitamin K antagonist oral anticoagulants (NOACs). For those without AF, the guidelines say anticoagulation with a vitamin K antagonist is reasonable for at least 3 months (class 2a).
Izumi noted that NOACs have been increasingly used at discharge for patients following bioprosthetic valve replacement “despite this being an off-label use for patients with sinus rhythm.”
But according to Manesh R. Patel, MD (Duke Clinical Research Institute, Durham, NC), in current United States practice, “many, if not most” patients undergoing bioprosthetic valve surgery do not receive anticoagulation in the first 3 months postprocedure. Going forward, clinicians need “to spend more time understanding who's at higher risk in that early period,” he told TCTMD. “There are patients having events there. This shows us at least that there's some data that this might be tolerated.”
The findings build off those seen in 2020 with the Korean ENAVLE study, which showed noninferiority of edoxaban to warfarin in this setting based on a primary endpoint of all-cause death, clinical thromboembolic events, or asymptomatic intracardiac thrombosis.
Speaking with TCTMD, B. Hadley Wilson, MD (Sanger Heart & Vascular Institute, Atrium Health, Charlotte, NC), past president of the American College of Cardiology, said the ENBALV findings may be the start of “a paradigm shift where we can see that that now it's opening the door for these new oral anticoagulant agents in post-op valve replacement to be used in the first 3 to 6 months, which is the highest period of time where you're going to have thromboembolic events.”
This is an attractive potential as NOACs are “a lot easier to use” than warfarin as there’s no need to measure prothrombin times and there’s fewer drug-drug interactions to worry about, he noted.
However, discussing the study during the session, Philippe Gabriel Steg, MD (Hôpital Bichat, Paris, France), said while ENBALV “properly addressed the issue of edoxaban versus warfarin” in the acute period following bioprosthetic valve surgery, the very low rate of events as well as the short TTR for warfarin mean the trial is not convincing enough to support the notion that the drugs are similar in this setting.
“With four primary outcome events in total, we cannot conclude that edoxaban was comparable to warfarin in ENBALV,” he said, also highlighting the difficulty of managing bleeding in the postoperative period. “Given these limitations, I think we have to accept that edoxaban did not provide comparable efficacy to warfarin. Warfarin treatment in the trial was poorly controlled, and it's a limitation of warfarin in this setting. But even accepting that, this was on the lower end of what is generally achieved.”
Similar Efficacy
For the study, Izumi and colleagues randomized 410 patients (mean age 73 years) who underwent mitral and/or aortic bioprosthetic valve replacement between May 2022 and January 2024 to receive at least 12 weeks of warfarin (once daily monitored by International Normalized Ratio) or edoxaban (once daily 30- or 60-mg).
Male patients made up 51.3% and 62.4% of the edoxaban and warfarin arms, respectively. About one in five patients had AF, and the vast majority of patients had aortic valve surgery. About one-third of the edoxaban arm received the 30-mg dose, with the remainder being prescribed 60-mg. TTR in the warfarin cohort was 19%.
There was no difference in the primary efficacy endpoint of stroke or systemic embolism between edoxaban and warfarin (0.5% vs 1.5%), but there was a numerically higher rate of major bleeding with edoxaban (4.1% vs 1.0%). Major bleeding events in the edoxaban group did not include any intracranial hemorrhage or fatal bleeding, but rather were pericardial (n = 2), surgical wound (n = 1), and urinary (n = 1). There was a single intracranial bleed in the warfarin arm that led to death, as well as one surgical wound bleed.
The net endpoint of stroke, systemic embolism, or major bleeding was not significantly different between the groups (4.6% vs 2.1%).
Izumi noted some limitations with the study. The researchers left the timing of anticoagulation initiation up to the surgeons, and this “may have influenced the incidences of the clinical events,” she said. Also, “TTR in the warfarin group was very short. However, we consider that this undertreatment with warfarin reflects the current clinical situation and is precisely the problem with warfarin.”
Specifically, Izumi explained, “hospital stays are now becoming shorter, . . . so it’s difficult to achieve TTR in a short hospitalization.”
While it’s “reasonable” to consider that patients might prefer edoxaban over warfarin “because of the lack of hassle,” Sten said that after leaving the hospital many of them go to cardiac rehab, where warfarin can be managed “more easily.”
Lastly, Izumi noted, the study did not include TAVI patients, and as such the findings cannot be applied to this population.
More Risk Stratification Needed
The findings will have implications for practice, since patients without AF have been shown to have an elevated risk of stroke and blood clots following bioprosthetic valve surgery, according to Patel. However, the “very few events” reported in ENBALV signal that although “this is a population that's at risk, they may be at a low risk,” he said.
“Our practice has to importantly improve the stratification of patients undergoing valvular surgery, specifically those that are undergoing bioprosthetic valvular surgery without known atrial fibrillation to see who's at risk for stroke and systemic embolism in that short-term period,” Patel added.
The current opportunity for researchers is to “take the large groups of patients that we're putting through these procedures and better understand their acute short-term stroke risks to [then] understand who's going to benefit the most from not just these therapies, but a variety of all these strategies,” he said.
Several risk scores exist or are in development, but none have so far stood out as being able to pinpoint the highest risk patients in this regard, Patel said.
Wilson said the higher-risk patients are likely those with any previous history of a thromboembolic event, even if not related to the valve, or an unexplained TIA “where you're concerned that there might be something going on that hasn't been diagnosed,” he added. Remote monitoring has gotten better with time to the point that it should be used to help guide these decisions, Wilson said.
“We need to further define that, but at the same time, this gives us more options,” he concluded, adding that “the next chapter” will be to conduct a similar study in TAVI patients to see whether they might benefit from NOAC therapy for 3-6 months instead of, say, dual antiplatelet therapy.
Izumi said this is only the beginning, as ENBALV is the “first evidence of the use of DOACs including patients with sinus rhythm, but the incidence of bleeding is high.” It’s important that further work identifies which patients are at high risk for bleeding with edoxaban, she said.
Yael L. Maxwell is Senior Medical Journalist for TCTMD and Section Editor of TCTMD's Fellows Forum. She served as the inaugural…
Read Full BioSources
Izumi C. Efficacy and safety of EdoxabaN in anticoagulant therapy after surgical Bioprosthetic vALVe replacement. Presented at: AHA 2024. November 17, 2024. Chicago, IL.
Disclosures
- The trial was funded by Daiichi Sankyo.
- Izumi reports receiving speaker honoraria from Daiichi Sankyo, Nippon Boehringer Ingelheim, and Novartis and research funding from Pfizer, LSI Medience, PPD-SNBL K.K., Abbott Medical Japan, Bristol-Myers Squibb, and Eli Lilly and Company.
- Steg reports receiving research grants from Amarin and Sanofi; serving on steering committees for Amarin, Amgen, AstraZeneca, Bayer, BMS, Idorsia, Janssen, Novartis, NovoNordisk, PhaseBio, Pfizer, and Sanofi; and serving as the CMO for Bioquantis.





Comments