Experts Debate: Should Cerebral Protection Be Used for All TAVRs?
Saif Anwaruddin says all patients should be protected, but Duane Pinto argues that the evidence supports a more selective approach.
DENVER, CO—There seems to be a consensus that cerebral embolic protection has a role to play for patients undergoing TAVR, but a debate held here last week at TCT 2017 underscores the remaining controversy over how extensively the devices should be used.
Saif Anwaruddin, MD (Hospital of the University of Pennsylvania, Philadelphia), maintained that the totality of the data—which demonstrates that protection devices are safe and effective—favors use of embolic protection in all patients undergoing TAVR.
“The question to ask is not, ‘Should we use embolic protection for all our patients or [employ] a selective strategy?’, but rather, ‘Why wouldn’t you use embolic protection in all your TAVR patients?’” he said during the debate.
On the other side, Duane Pinto, MD, MPH (Beth Israel Deaconess Medical Center, Boston, MA), argued that, even though protection devices have been shown to efficiently collect debris and reduce evidence of emboli on brain imaging, inconclusive evidence from clinical trials supports a more selective approach.
“Stratification based on risk factors may be the more appropriate strategy,” he said.
Routine Use in All Patients
Anwaruddin said certain common misconceptions needed to be addressed when discussing routine use of embolic protection during TAVR. Those were:
- With newer-generation TAVR valves and greater operator experience, strokes will become less of a concern.
- Available trial data do not support the benefit of embolic protection for reducing stroke.
- It isn’t worth treating all patients to prevent a low-frequency event.
Stroke remains a problem, he said, pointing to the 5.6% rate of stroke in the protection arm of the SENTINEL trial and the 4.6% rate among patients in whom a protection device was not used in a propensity-matched analysis. In the original PARTNER trial, he noted, the stroke rate was about 5.5%. Acknowledging that there were differences in how strokes were adjudicated across studies, Anwaruddin said, “The point is: I don’t think we’ve really progressed all that much in all that time. So yes, stroke is still a concern.”
As for whether cerebral embolic protection devices do what they’re supposed to do, he pointed out that debris that otherwise would have gone to the brain is captured by filters in 100% of cases. “So if you’re talking about a selective strategy, you’re basically saying that I’m okay with having some ischemic hits in some of my patients, even though it may not manifest as strokes in all patients,” he said.
Why wouldn’t you use embolic protection in all your TAVR patients? Saif Anwaruddin
He also argued that the totality of the data indicates that the devices effectively reduce stroke. The SENTINEL study did not show a significant improvement in 30-day stroke with protection (5.6% vs 9.1%; P = 0.25), but Anwaruddin said it would be more relevant to focus on the periprocedural period. In the first 3 days, patients who received the Sentinel filter device (Claret Medical) had a significantly lower rate of stroke (3.0% vs 8.2%; P = 0.05).
That trial has been criticized for being underpowered, but a pooled analysis of the SENTINEL, CLEAN-TAVI, and MISTRAL-C trials—all evaluating the Sentinel device—showed a benefit of using embolic protection, Anwaruddin said. He added that another meta-analysis by Gennaro Giustino, MD (Icahn School of Medicine at Mount Sinai, New York, NY), and colleagues that included two additional trials with different devices also showed a benefit in terms of a composite of death or stroke.
Moreover, a propensity-matched analysis showed that embolic protection with the Sentinel device was associated with fewer overall strokes (1.4% vs 4.6%; P = 0.03) and a lower rate of all-cause mortality/all strokes (2.1% vs 6.8%; P = 0.01) at 7 days. “This really flies against the concept of using a selective strategy . . . because the only risk factor [for poor outcomes] is really not using the device,” Anwaruddin said.
Capping off his argument for routine use of embolic protection in all patients undergoing TAVR, Anwaruddin cited the additional short- and long-term costs associated with periprocedural stroke.
Routine Use Not Justified
Pinto was not convinced, joking, “Your conclusions were great, if only they were right.”
The question is whether existing outcomes support embolic protection in TAVR becoming the standard of care, he said, pointing out that protection devices have not been shown to reduce clinical stroke in a randomized trial.
Your conclusions were great, if only they were right. Duane Pinto
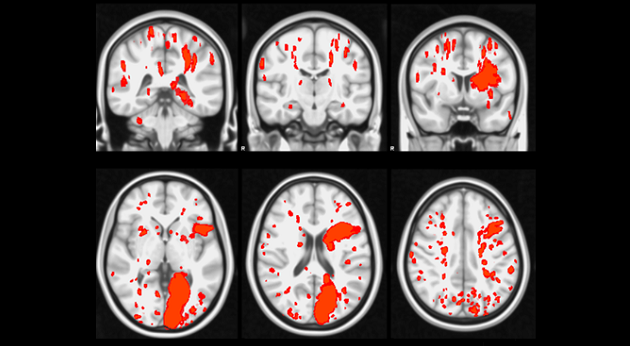
Though there is evidence that the devices have a beneficial impact on surrogate endpoints, including white matter lesions on diffusion-weighted MRI, there is not sufficient evidence that those benefits translate into a reduction in clinical stroke, Pinto indicated, noting that many post-TAVR lesions resolve over time.
Supporting a disconnect between white matter lesions on MRI and clinical stroke, Pinto cited a meta-analysis showing no impact of protection on overt stroke.
Pinto also raised the possibility that placement of embolic protection devices could be causing some strokes, saying that about 5% of patients treated with one of the filters still had a stroke in the protected area. And, he said, the 30-day stroke rate in the protection arm of the SENTINEL trial (5.6%) was higher than the weighted average of about 4.5% across studies of contemporary TAVR valves. “So either it’s from placement of the device or the device was incompletely protecting those areas,” Pinto said.
Thus, he concluded, “before we can advise routine use [of protection devices] amongst all TAVR patients, we need actual randomized evidence that they prevent stroke. And given the prevalence of stroke in protected areas, we should know whether it’s because of the device or in spite of the device.”
Cost Is an Issue
During a panel discussion following the debate, several physicians said cost is an issue when considering use of cerebral embolic protection during TAVR.
Mohamed Abdel-Wahab, MD, PhD (Heart Center, Segeberger Kliniken, Bad Segeberg, Germany), said the cost of the devices is not negligible. And because the filters cannot be easily placed in all anatomic variants, he added, there will need to be some alterations to the devices before they can become standard of care.
Others downplayed the cost issue. Ganesh Manoharan, MBBCh, MD (Royal Victoria Hospital, Belfast, Northern Ireland), said he uses embolic protection in certain high-risk patients—those undergoing a valve-in-valve procedure, those with evidence of thrombus in the left atrial appendage, or those with friable tissue on the aortic valve. But he argued that if companies packaged embolic protection devices with their TAVR systems and sold those packages at the same price as the TAVR system alone, physicians would use protection more widely. “If the issue here is cost and the cost is taken out of the equation, then you would use it,” he said. “It’s an easy device to use.”
Torsten Vahl, MD (NewYork-Presbyterian/Columbia University Medical Center, New York, NY), said he understands the concerns about cost. But, he added, stroke is the worst event that can occur following TAVR and there are no reliable predictors of which patients are most at risk. “So, therefore, I also subscribe currently to using [embolic protection] in all patients where anatomically we think it’s feasible,” he said.
In a show of hands following the debate and panel discussion, the audience appeared to favor more routine use of embolic protection.
Photo Credit: Leon MB. Embolic Protection Devices For TAVR Procedures: Lessons Learned From SENTINEL and Other Experiences. Presented at TCT 2017.
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Anwaruddin S. Point: a balanced look at all the data favors cerebral protection in all TAVR patients. Presented at: TCT 2017. November 1, 2017. Denver, CO.
Pinto DS. Counterpoint: clinical trial results are inconclusive and systematic use of cerebral protection during TAVR is unwarranted. Presented at: TCT 2017. November 1, 2017. Denver, CO.
Disclosures
- Anwaruddin reports receiving consulting fees/honoraria from Edwards Lifesciences and Medtronic and institutional grant support from Edwards Lifesciences.
- Pinto reports receiving consulting fees/honoraria from Medtronic, Medicure, Chiesi, and Abiomed, as well as royalty income from UpToDate.


Comments