FFR During Angiogram Not Beneficial in Chest Pain Patients: RIPCORD 2
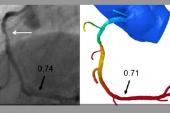
During the diagnostic angiogram, a physiologic assessment of all epicardial vessels was cost neutral but didn’t improve QoL.

A routine strategy that assesses function of all epicardial vessels at the time of diagnostic angiography in patients with new-onset chest pain doesn’t cost any more than conventional diagnostic angiography, but the systematic physiologic assessment does not translate into meaningful benefits, according to the results of the RIPCORD 2 study.
Overall, there were no improvements in patient quality of life or angina status at 1 year with the routine use of fractional flow reserve (FFR), and its use was associated with longer procedures, greater use of radiation and contrast, and a higher rate of complications.
The results from RIPCORD 2, he said, are consistent with the findings from the FORECAST trial, which was presented last year. In FORECAST, up-front use of CT-derived FFR in patients with new-onset chest pain did not translate into an economic benefit.
“That, too, was negative,” said Curzen. “I think we’re beginning to see that while vessel-specific ischemia in the form of pressure-wire assessment is a really good tool once a person has been allocated to PCI, it might not be necessary when you’re at the diagnostic stage deciding whether someone should have medical therapy, PCI, or CABG. In fact, it doesn’t seem to be of any benefit at all.”
For Stefan James, MD, PhD (Uppsala University Hospital, Sweden), who commented on the study for TCTMD, the rationale for RIPCORD 2 makes intuitive sense given that operators are looking to collect as much diagnostic information as possible. However, he added, the trial clearly shows that FFR is unnecessary in this setting.
“We know that a physiological measurement is helpful when we’re about to decide whether or not to perform a PCI,” said James, “but there is a risk that we will start collecting more and more diagnostic measurements in patients without a clear indication for PCI. FFR might be underutilized in many cases, but it might also be overutilized. This study suggests it’s important to use when you’re in doubt, and if you want to avoid a procedure you intended to do, but it doesn’t help to guide you when adding it to a diagnostic procedure.”
No Change in QoL, Outcomes
In presenting the results during the Hot Line session at the European Society of Cardiology Congress 2021, Curzen highlighted the first RIPCORD study, which was published in 2014. There, investigators showed that use of FFR led to a change in the management strategy for roughly 25% of patients undergoing PCI when compared with coronary angiography alone. He also pointed out that the landmark FFR studies—DEFER, FAME, and FAME-2—compared FFR versus coronary angiography in patients already committed to PCI. In RIPCORD 2, however, investigators took the use of FFR back one step and sought to assess the value of systematic FFR at the stage of diagnostic angiogram.
We don’t need to know vessel-specific ischemia in order to make a management plan above and beyond just looking at the angiogram. . . . That will be a very unattractive, unpalatable fact for some interventional cardiologists. Nick Curzen
The study included 1,100 patients undergoing diagnostic coronary angiography at 17 UK centers for stable angina or NSTEMI. In the angiography arm, the assessment and management of patients was based on the angiogram alone while the FFR strategy included the physiologic assessment plus angiography to guide management decisions. In the FFR arm, operators performed pressure-wire assessment in a median of four coronary vessels.
For the two co-primary endpoints—total hospital costs and quality of life assessed by the EQ-5D visual analogue scale at 1 year—there was no significant difference between the two strategies. There was also no difference in the risk of major adverse cardiovascular events (death, stroke, MI, or unplanned revascularization) between the two approaches. Additionally, FFR plus angiography did not alter the distribution of optimal medical therapy, PCI, or CABG surgery.
Procedural times were longer in the FFR group (mean 42.4 vs 69.0 min; P <0.001), contrast use was significantly greater (mean 146.3 vs 206.0 mL; P <0.001), and radiation doses were higher (mean 5,029 vs 6,608 cGy/cm2; P <0.001). The complication rate in the FFR arm was 1.8%, mainly the result of dissections.
The present study shows that a routine FFR assessment at the time of diagnostic angiography in chest-pain patients provides no overall advantage over angiography alone, said Curzen. Citing the results from ISCHEMIA, where anatomy, but not ischemic severity, was predictive of clinical events, as well the 5-year outcomes from SCOT-HEART, where the use of CT angiography lowered the risk of CHD death and nonfatal MI, Curzen said the evidence is lining up to support operators using angiography to allocate patients to optimal medical therapy (OMT), PCI, or CABG surgery, “as long as everybody gets OMT.”
However, he pointed out that the uptake of pressure-wire assessment of coronary lesions is incompatible with the wealth of evidence showing its benefit for guiding revascularization in patients undergoing PCI. He cautioned that he would not like to see RIPCORD 2 misinterpreted. “I suspect that people who were underutilizing the pressure wire even with its evidence base will potentially use this result as an excuse to do even less,” said Curzen. “That’s not really what we hope happens as a result of RIPCORD 2.”
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Curzen N. RIPCORD 2: Does routine pressure wire assessment influence management strategy of coronary angiography for diagnosis of chest pain. Presented at: ESC 2021. August 29, 2021.
Disclosures
- Curzen reports research contracts with Boston Scientific, HeartFlow, Beckman Coulter and speaking fees from Boston Scientific, Abbott, and HeartFlow.
- James reports no relevant conflicts of interest.



Comments