No Cost Savings With Routine FFRCT for New-Onset Chest Pain: FORECAST
FFRCT did reduce the use of invasive angiography, but the savings weren’t enough to offset the up-front costs of testing.
Contrary to the opinion of the UK’s National Institute for Health and Care Excellence (NICE), up-front use of CT-derived fractional flow reserve (FFRCT) in patients with new-onset chest pain will not save the National Health Service (NHS) millions of pounds each year.
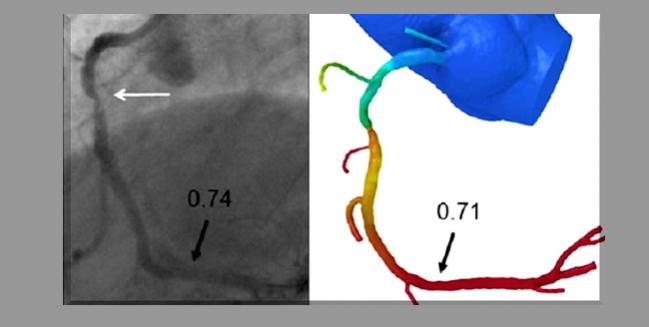
That’s the takeaway from FORECAST, a new economic analysis that addressed whether routine physiologic testing with FFRCT (HeartFlow), calculated after CT angiography or other tests, reduced resource utilization when compared with the typical clinical assessment of chest pain. Although the information gleaned from FFRCT significantly reduced the rate of invasive angiography by 22% compared with usual care, the overall costs of the strategies were similar, according to researchers.
“That’s quite a major difference to how NICE had projected it from the observational data,” said lead investigator Nick Curzen, BM, PhD (University Hospital Southampton NHS Foundation Trust, England), last week in a late-breaking clinical science session during TCT Connect 2020.
In 2017, based on observational studies, NICE issued a “technology appraisal” in support of FFRCT, explained Curzen. According to NICE, the use of FFRCT would save £214 per patient and that by “adopting this technology, the NHS in England may save a minimum of £9.1 million by 2022 through avoiding invasive investigation and treatment.”
The observational studies underpinning that recommendation included PLATFORM, where an FFRCT-guided strategy in patients with suspected CAD reduced the need for invasive coronary angiography compared with routine care. Data from the ADVANCE registry showed that FFRCT led physicians to rethink their initial treatment approach (based on CT angiography alone) in roughly two-thirds of patients, while RIPCORD showed that FFRCT changed the treatment strategy in 36% of patients initially screened with CT angiography.
For that reason, the FORECAST investigators focused on resource utilization for their primary endpoint.
“The real question, based on the observational data, wasn’t so much would it reduce angiography rates without increasing rates of clinical events or coronary revascularization, because these things have been consistent in the observational studies,” said Curzen. “It was more whether the strategy of FFRCT was cost-effective in these patients.”
The study included 1,400 patients presenting to rapid-access chest-pain clinics at 11 UK centers. In the reference group, patients were treated with usual care, with more than 60% undergoing CT angiography alone as the initial test and the remaining getting stress echocardiography (14.7%) or exercise ECG (10.0%) for their initial workup. In the study arm, patients underwent CT angiography and then had FFRCT assessed if they had a coronary stenosis > 40% in at least one major epicardial vessel. In the test arm, 31.5% of patients with chest pain had an initial FFRCT performed following CT angiography.
At 9 months, more noninvasive and invasive testing occurred in the usual-care arm, with 175 of 700 patients sent for invasive angiography. In the test group, 136 of 699 patients had a coronary angiogram. Overall, the FFRCT strategy reduced the number of invasive angiograms by 14% versus the reference group (P = 0.02), with 22% fewer patients undergoing invasive angiography (P = 0.01).
Despite the reduction in invasive angiography, there was no significant difference in resource utilization between the two strategies, including no difference in total costs (£1,491.46 with usual care vs £1,605.50 with FFCRT; P = 0.962). Regarding secondary clinical endpoints, there were no differences in risks of MACCE or coronary revascularization between the two approaches and no differences in quality of life or angina status at 9 months.
Avoiding Caths for 1 in 5 Patients
Moderating the session, Gregg Stone, MD (Icahn School of Medicine at Mount Sinai, New York, NY), said FORECAST is the first randomized trial to explore the hypothesis raised in PLATFORM, namely that use of FFRCT could reduce costs relative standard care. While the trial failed on that front, “it would certainly seem that avoiding cath in 22% of patients is desirable,” he said. Stone asked Curzen’s opinion on the best way to manage patients with chest pain in light of these new data.
“To me, what [FORECAST] means is that when we’re planning to take care of people, an up-front CT [coronary angiography] test is a very valuable way of deciding whether they should be committed to optimal medical therapy and anti-anginal therapy,” he said. “I suspect that a better strategy than immediately using FFRCT up front would be to wait and see if people’s angina settles after they’ve been on that medical therapy. If it hasn’t, then deploy FFRCT, which you can do retrospectively without doing another test to see if the patient needs revascularization and if so, to plan the strategy.”
William Fearon, MD (Stanford University School of Medicine, CA), believes the results are informative in light of ISCHEMIA, particularly the finding that ischemic burden was not predictive of clinical events or treatment benefit. As several experts noted at the time, it may be possible to skip noninvasive stress imaging for CT angiography to rule out left main disease, and adding FFRCT would only further support that approach, said Fearon.
In terms of the lack of financial benefit, Fearon pointed out that 66% of patients in the usual-care arm were eventually screened with CT angiography, meaning only one-third of patients with new-onset chest pain were managed differently than those in the test group.
Curzen said they anticipated high utilization rates of CT angiography following a 2016 update from NICE that recommend the noninvasive test as a first-line strategy for patients with new-onset chest pain. He pointed out, however, that FORECAST was not designed to be a comparison of FFRCT with CT angiography, but rather an assessment of whether FFRCT was a cost-effective approach.
“We knew that the amount of [CT angiography] in the reference arm would increase throughout the recruitment because the CG95 guideline had changed just before we started recruiting,” said Curzen. “But I don’t think it really affects the results of the trial. What the study is telling us is that the addition of FFRCT on top of [CT angiography], or any other test, was not cost-dominant.”
In a press conference, Curzen told TCTMD they performed several sensitivity analyses looking at different price points for FFRCT to see at what cost it might lead to savings, but none made sense from a financial perspective. In essence, the reduction in invasive angiography was not large enough to take into account the up-front cost of FFRCT.
“We can reach a point where it saves money, but probably not by using it so freely,” said Curzen.
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Curzen N, on behalf of the FORECAST investigators. Fractional flow reserve derived from computed tomography coronary angiography in the assessment and management of stable chest pain. Presented at: TCT 2020. October 16, 2020.
Disclosures
- Curzen reports institutional grant/research support from Boston Scientific, HeartFlow, and Haemonetics; and consulting fees/honoraria from Abbott Vascular, Boston Scientific, HeartFlow, and Haemonetics.
- Fearon reports institutional grant/research from Abbott Vascular, Medtronic, and Edwards Lifesciences; consulting fees/honoraria from CathWorks; and equity/stocks from HeartFlow.
- Stone reports speaker honoraria from Cook; consulting to Valfix, TherOx, Robocath, HeartFlow, Gore, Ablative Solutions, Miracor, Neovasc, Abiomed, Ancora, Vectorious, and Cardiomech; and equity/options from Ancora, Qool Therapeutics, Cagent, Applied Therapeutics, Biostar family of funds, SpectraWave, Orchestra Biomed, Aria, Cardiac Success, and Valfix.


Comments