Five-Year Follow-up Reassures on Severe Patient-Prosthesis Mismatch in TAVI
Predicted PPM picked up fewer “severe” cases than did measured PPM, providing some validation for VARC-3 recommendations.
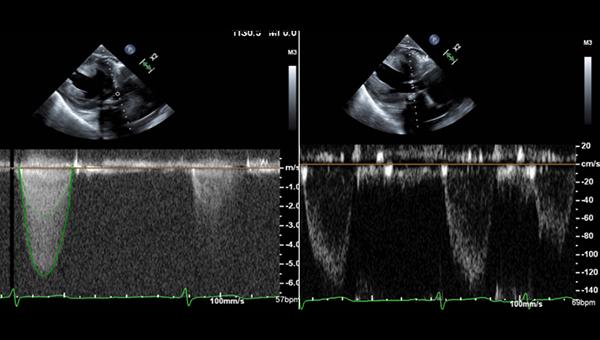
Photo Credit: Adapted from Siddiqullah S. Case of a patient prosthesis mismatch leading to early transcatheter aortic valve degeneration. Presented at: TVT 2023. Phoenix, AZ.
PHOENIX, AZ—An in-depth analysis of patient-prosthesis mismatch (PPM) following TAVI, primarily with a balloon-expandable valve, in patients at mostly intermediate or high risk for aortic valve surgery indicates that mortality at 5 years is no higher with severe PPM than with moderate or no PPM.
The lack of an association in this all-comers population was seen both for measured PPM and predicted PPM, and for native TAVI procedures as well as valve-in-valve (ViV) TAVI, said Karim Al-Azizi, MD (Baylor Scott & White Health, Plano, TX), who reported the real-world, multicenter analysis at the TVT 2023 meeting last week.
Moreover, measured PPM tended to overestimate the problem, categorizing more PPM as “severe” than did predicted PPM and thereby validating the latter, he noted, which is what’s recommended by the Valve Academic Research Consortium 3 (VARC-3) for estimating PPM in advance of a procedure.
“Severe measured PPM and predicted PPM in native TAVI or ViV TAVI was not associated with worse outcomes compared to moderate or no PPM at 5 years,” Al-Azizi summarized. “Further subanalyses are underway to delineate potential predictors of mortality and PPM, as well as comparisons between different prosthesis platforms.”
PPM is defined by an effective orifice area (EOA) considered too small in relation to a patient’s body surface area, based on concerns that the incongruity will cause hemodynamic problems for the patient when the new valve is in place. In surgically treated patients, PPM has been linked to adverse clinical outcomes following surgical aortic valve replacement: whether TAVI valve PPM carries the same risks has been disputed.
These findings, from multiple centers within a single health system, closely confirm what was also seen in an echo core-lab analysis of the PARNTER 2A trial, said Philippe Pibarot, DVM, PhD (Laval University, Canada), one of the leading researchers on the topic of PPM. His conclusion from Al-Azizi’s registry results is that true, severe PPM likely still confers adverse prognosis, but that this phenomenon is becoming increasingly rare.
“This study tells me that we are on a good path with the improvement of the hemodynamics of the valve, both on the surgical side and the TAVI side,” Pibarot, who was also a panelist for Al-Azizi’s presentation, told TCTMD. “I think severe PPM is becoming rare except in patients with a very small annulus or hostile anatomy. There are still a few patients where we would have to pay attention to that and maybe the surgeon, if the patient goes to SAVR will need to do a root enlargement, but this is really in highly selected cases when you can predict there is a risk of severe PPM.”
Predicting a Mismatch
Al-Azizi and colleagues looked retrospectively at all patients who’d undergone a TAVI procedure at one of six hospitals in the Baylor Scott & White Healthcare System in Texas between 2012 and 2021. Nearly 44% of patients were female, 36.8% had a body mass index (BMI) over 30, and 44.3% were high risk while 39.4% were intermediate risk. Almost three-quarters of patients were treated with a balloon-expandable valve (Sapien, Sapien XT, or Sapien 3; Edwards Lifesciences).
PPM values were stratified as nonsignificant, moderate, or severe using the indexed effective orifice area (EOAi, based on EOA/body surface area). Lower cutoff adjustments were used for patients with a BMI ≥ 30. Measured EOA was obtained from transthoracic echocardiography at discharge using the continuity equation, whereas predicted EOA was obtained from published predictive tables for each model and size of transcatheter valve.
This study tells me that we are on a good path. Philippe Pibarot
Comparing measured versus predictive EOA and EOAi, as well as PPM, was telling, said Al-Azizi. Across the board, measured EOA and EOAi were significantly greater than the predicted values, yielding significantly higher rates of severe measured PPM, both unadjusted and adjusted for BMI, than those PPM results derived from the predicted equations. Of note, the rate of severe predicted PPM, adjusted for BMI, was just 1.3%.
Reassuringly Rare
Neither severe PPM or any PPM, whether measured or predicted, was associated with increased mortality out to 5 years, a finding that held true for native TAVI and ViV.
That message should be reassuring for TAVI operators concerned about the signal of worse outcomes associated with PPM in the surgical literature, and for referring cardiologists, who might have questions for proceduralists about whether they should be worried about valve gradients following a patient’s procedure, particularly if that patient is older and higher risk for surgery, said Al-Azizi.
For younger, lower-risk patients, he cautioned, the calculus shifts somewhat. While older patients at higher risk made up most of this cohort, in younger, healthier subjects, the focus would appropriately be on lifetime management. That means implanting a device that provides the largest EOA in order to leave the door open to future reinterventions.
Pibarot pointed out that while the PARTNER 2A analysis suggested severe PPM tended to be more of a problem with SAVR-treated patients than with TAVI, surgical bioprostheses and techniques have also been improving, such that severe PPM is less common in surgically treated patients, too.
One issue, Pibarot noted following Al-Azizi’s presentation, is that measuring EOA is “challenging” because it is often performed when patients are in a low-flow state.
“The majority of the patients post-TAVI, they don’t have a normal flow, and so the EOA that we measure is often pseudo-severe PPM . . . with no impact on outcomes,” he said. “That’s why the predicted PPM—and I’m really happy that you did that—is interesting, because it is independent of the flow condition. It really gives you the hemodynamic fingerprint of the valve versus the body size. And you can see, when you use this method and you correct for BMI using the VARC-3 definition, you have [a severe-PPM rate of] 1%, meaning that the risk factor, which is the true severe PPM, almost does not exist anymore with the current TAVI. [This] is good news, and that’s why you have no impact on mortality.”
Shelley Wood was the Editor-in-Chief of TCTMD and the Editorial Director at the Cardiovascular Research Foundation (CRF) from October 2015…
Read Full BioSources
Al-Azizi K. 5 year outcomes of TAVI patients with prosthesis-patient mismatch. Presented at: TVT 2023. June 9, 2023. Phoenix, AZ.
Disclosures
- Al-Azizi reports consulting fees/honoraria from Edwards Lifesciences, Medtronic, Boston Science, and Abbott.





Comments