Invasive Testing Safely Diagnoses Microvascular Dysfunction in ANOCA
(UPDATED) Finding the cause of angina in patients without obstructed coronaries can reassure patients and lead to tailored therapy.

Invasive coronary functional testing to identify the cause of angina in patients with nonobstructive coronary artery disease (ANOCA) can be performed safely at both experienced and less-experienced centers, according to a new study.
The invasive testing was done at 15 tertiary and nontertiary hospitals in the Netherlands and resulted in a high rate of diagnosis—the predominant ANOCA endotype was spasm—plus low rates of major and minor complications, reported researchers from the Netherlands Registry of Invasive Coronary Vasomotor Function Testing (NL-CFT).
Senior investigator Peter Damman, MD, PhD (Radboud University Medical Center, Nijmegen, the Netherlands), said the study confirms that testing can be done safely and that there is a high diagnostic yield when it is carried out. “The safety is important as this is a known hurdle to perform [coronary function testing] in nonexperienced centers,” he told TCTMD.
In the 2024 European Society of Cardiology (ESC) guidelines for chronic coronary syndromes, invasive coronary angiography with the availability of functional testing is recommended to confirm or exclude obstructive coronary disease or ANOCA in patients with an uncertain diagnosis on noninvasive imaging (class I, level of evidence B). Functional testing is also recommended to define ANOCA and to identify potentially treatable endotypes (class I, level of evidence B).
In the US, invasive functional testing is also considered reasonable to improve the diagnosis of patients with persistent chest pain without coronary obstruction (class 2a, level of evidence B).
Prior studies have shown that roughly 50% of patients who undergo coronary angiography for angina have no coronary obstruction warranting revascularization, said Damman. “However, this is only when angiography is performed,” he said. “In those patients with angina in which no angiography is performed—for example, because they respond well to medical therapy—the true prevalence is unknown.”
Vijay Kunadian, MBBS, MD (Newcastle University Translational and Clinical Research Institute, Newcastle upon Tyne, England), who was involved in drafting the ESC chronic coronary syndrome guidelines around ANOCA/ischemia with nonobstructive coronary arteries (INOCA), said these patients have historically been told there was nothing wrong with them or there was little the doctor could do.
“That’s often the dialogue that comes during the consultation, but now we’re learning that this is not a benign condition,” she told TCTMD. “It affects women more than men and women continue to have a lot of symptoms, which can be debilitating.”
There are survey data, Kunadian added, describing the large impact of ANOCA/INOCA on physical functioning, mental health, and quality of life. Instead of counseling the patient that there is nothing wrong, the onus is on physicians to push beyond looking for a coronary stenosis only. “You don’t just stop at angiography,” she said. “You have to go and look for the microvascular dysfunction.”
If physicians do look, they’ll find it in a large percentage of patients, as the NL-CFT study confirms, she said.
Harmony Reynolds, MD (NYU Langone Health, New York, NY), another cardiologist with expertise in ANOCA/INOCA, said the low complication rate with functional testing lines up with their clinical experience.
“This is safe testing, and it's good for everybody who does invasive angiography to be familiar with this testing,” she told TCTMD. “They can have patients come into the cath lab, looking for a diagnosis, and then exit with a diagnosis.”
Low Rate of Complications
The study, led by Caïa Crooijmans, MD (Radboud University Medical Center), and published last week in JAMA Cardiology, included 1,207 patients (mean age 60 years; 81% female) treated at hospitals participating in NL-CFT. One-third of patients were treated at tertiary centers, which was defined as having performed more than 100 coronary function tests and currently serving as a referral hospital with a specialized ANOCA outpatient clinic. More than 90% of patients reported angina symptoms of pain, pressure, or chest tightness, while 56% reported shortness of breath.
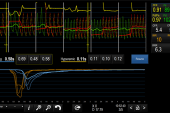
Intracoronary acetylcholine was used to provoke coronary spasm (administered at 2, 20, 100, and 200 µg), while resting and hyperemic measurements with intravenous adenosine were used to measure coronary flow reserve and microvascular resistance. Conclusive results of both parts of the functional testing were available for 95% of patients.
This is safe testing, and it's good for everybody who does invasive angiography to be familiar with this testing. Harmony Reynolds
In total, 78% of patients had an abnormal test result: 9% had coronary microvascular dysfunction (CMD), 31% had isolated epicardial spasm, 12% had epicardial spasm and CMD, 17% had isolated microvascular spasm, and 9% had microvascular spasm and CMD. Vasomotor dysfunction was more frequently diagnosed at tertiary-care centers (86% vs 71%; P < 0.001).
The rate of major complications was 0.9%. There were three coronary dissections or other vascular complications, two cases of ventricular tachycardia > 30 s or ventricular fibrillation, and two cases of hemodynamic instability, among others. The risk of major complications did not differ between tertiary and nontertiary centers (1.3% vs 0.6%; P = 0.22).
Atrial fibrillation requiring conversion, a minor complication, occurred in 10 patients (0.8%), with no significant difference between centers.
Tailoring Therapy
The identification of ANOCA endotypes can lead to more personalized patient care, said Damman, although treatment is still mainly based on expert consensus and smaller studies. In the 151-patient CorMicA study, for example, tailoring angina medications to a diagnosis of microvascular dysfunction or vasospasm improved symptoms and quality of life over 6 months of follow-up, he noted.
With a complication rate at less than 1%, patients and physicians alike shouldn’t fear these invasive tests, said Kunadian.
“You’ve given the patient a diagnosis rather than telling them there’s nothing wrong with them,” she said, noting that there are psychological benefits to the diagnosis in addition to allowing for individualized treatment.
You don’t just stop at angiography. You have to go and look for the microvascular dysfunction. Vijay Kunadian
Reynolds said that she is frequently referred patients with unexplained chest pain seeking a second opinion.
“In my own experience, I find that people definitely feel better if you give them a specific diagnosis,” she said. “I often see people who have seen other cardiologists and are still confused about why their symptoms exist and whether they’re heart-related or not. I find it’s really helpful to people to know that their symptoms are cardiac.”
In the ESC guidelines, calcium channel blockers are recommended to control symptoms and to prevent ischemia and potentially fatal complications in ANOCA/INOCA patients with isolated vasospasm (class I, level of evidence A). Nitrates are also an option to prevent recurrent episodes (class II, level of evidence B). In those with microvascular angina, beta-blockers should be considered for symptom control (class IIa, level of evidence B). In those with overlapping endotypes, the guidelines recommend combination therapy with nitrates, calcium channel blockers, and other vasodilators (class IIb, level of evidence B).
Damman said that more studies still needed, and next steps should focus on improving evidence-based tailored treatments.
At the upcoming American College of Cardiology Scientific Session, results of the WARRIOR trial will be presented, noted Reynolds. The event-driven, multicenter, randomized trial is comparing intensive medical therapy versus usual care in women with suspected INOCA. Additionally, Reynolds is involved in a study looking into the benefits of virtual cardiac rehabilitation versus usual care in patients with ANOCA/INOCA.
“There are lots of different avenues for treatment being looked into,” said Reynolds.
In terms of performing invasive functional testing outside experienced centers, Kunadian said PCI is routinely performed in nontertiary centers throughout the UK. No center should be performing angiography without the ability to provide complete diagnostic assessments, including invasive functional testing, she added.
“It’s not rocket science,” she said. “We’ve been doing angiograms for a very long time. It’s just an extra wire down the coronary artery [for functional testing].”
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Crooijmans C, Jansen TPJ, Meeder JG, et al. Safety, feasibility, and diagnostic yield of invasive coronary function testing: Netherlands Registry of Invasive Coronary Vasomotor Function Testing. JAMA Cardiol. 2025;Epub ahead of print.
Disclosures
- Damman reports grants from Abbott and Philips.




Comments