Lariat LAA Ligation Doesn’t Boost Effect of AF Ablation: aMAZE Trial
The added procedure failed to significantly reduce atrial arrhythmia recurrence in patients with persistent AF.
In patients with persistent atrial fibrillation (AF) undergoing initial catheter ablation, the addition of left atrial appendage (LAA) ligation with the Lariat system (AtriCure) did not improve arrhythmic outcomes over pulmonary vein antral isolation alone, results of the randomized aMAZE trial show.
“The Lariat system appears to be safe and successfully excludes the left atrial appendage in this first prospective, rigorous, and independently monitored clinical trial evaluating the [system],” David Wilber, MD (Loyola University Chicago, IL), reported recently at the virtual American Heart Association (AHA) 2021 Scientific Sessions.
The rate of freedom from documented atrial arrhythmias without a change in antiarrhythmic drug therapy at 1 year, however, was not significantly higher when the Lariat was added to the ablation procedure (64.3% vs 59.9%). Though subgroup analyses suggest that patients with early persistent AF and larger left atrial volumes might benefit from LAA ligation, “further investigation is required to verify these exploratory observations,” Wilber said.
Looking for Answers in Persistent AF
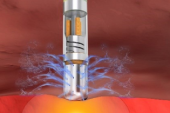
Wilber pointed out that results of pulmonary vein antral isolation (PVAI) have been suboptimal in studies of patients with persistent AF, leading researchers to look for adjunctive strategies to improve outcomes. Because the LAA is thought to be involved in the maintenance of persistent and long-standing persistent AF, aMAZE investigators hypothesized that ligating the appendage with the Lariat system would decrease atrial arrhythmia recurrence in this hard-to-treat population.
The aMAZE trial, designed as an investigational device exemption (IDE) study to evaluate the Lariat system for this particular purpose, was conducted at 53 US sites, enrolling 610 patients (mean age 67; 27% female) with symptomatic persistent and long-standing persistent AF who had failed antiarrhythmic drug therapy and were slated for initial catheter ablation. They were randomized 2:1 to LAA ligation with the Lariat on top of PVAI or to PVAI alone. In all patients, PVAI was performed with radiofrequency, contact force sensing, and irrigated tip catheters following a strict protocol: validation of pulmonary vein isolation with adenosine, a cavo-tricuspid isthmus line in all patients, and consideration of ablation of additional sites in the left atrium as a protocol deviation.
The Lariat procedure had high technical success, with effective LAA ligation (residual communication smaller than 1 mm) achieved in 87% of patients after the procedure and in 85% at 1 year.
The rate of the primary safety endpoint, a composite of post-Lariat serious adverse events within 30 days, was 3.4%, coming in below the 10% performance goal. The most common events were bleeding (2.2%), although three patients (0.8%) had serious injuries to the heart/related structures requiring surgery.
The primary effectiveness endpoint was freedom from documented atrial arrhythmias without changes in antiarrhythmic drug therapy at 1 year, and the absolute 4.3% higher rate in the Lariat arm did not meet the threshold for superiority. The Bayesian posterior probability was 0.835, short of the 0.977 needed to establish success.
Prespecified subgroup analyses hinted at a benefit from adding LAA ligation in patients with a short duration of persistent AF (7 days to less than 6 months) and a large LA volume (133 cm3 or greater), although those should be considered exploratory.
Questions Remain
“The aMAZE trial is a well-designed study that supports durable left atrial appendage mechanical exclusion with the Lariat device,” discussant Usha Tedrow, MD (Brigham and Women’s Hospital, Boston, MA), commented after Wilber’s presentation. The add-on procedure didn’t result in improved arrhythmic outcomes in the overall population, “though subgroups may benefit,” she said.
There was reason to believe that LAA ligation would have some utility in this setting, Tedrow indicated, pointing to smaller studies demonstrating lower rates of arrhythmia recurrence in patients undergoing LAA isolation on top of standard ablation, albeit with a higher thrombus risk.
Tedrow provided three explanations for why the LAA might be involved in the initiation and continuation of persistent AF: autonomic ganglia are usually present along the groove between the left superior pulmonary vein and the appendage; the appendage is near the ligament of Marshall, which is an “important substrate” for AF; and automatic tachycardias from the appendage may trigger AF.
Nonetheless, despite the reasonable safety and durable closure with the Lariat system, the primary endpoint failed to show a significant advantage for LAA ligation, and some important questions remain unanswered, Tedrow said. They center on whether safety could be enhanced with newer techniques for pericardial access, what impact the strict PVAI protocol and high success rates in the control arm had on the study’s results, whether there are any insights on voltage mapping to explain the lack of benefit in the treatment arm, and whether other adjunctive ablation strategies could enhance efficacy.
During a panel discussion following the presentation, Wilber said one potential explanation for why the trial wasn’t successful was the better-than-expected results from PVAI alone in the control arm. Another was the bias in enrollment toward patients with early persistent AF, who made up 79% of the study population.
What all this adds up to is a little more uncertainty than expected, emphasizing the importance of randomized trials, Wilber said. “It may not be the same strategy for everybody with persistent atrial fibrillation. Some patients might do fine with pulmonary vein isolation alone, as we saw in this trial,” whereas other patients with identifiable features like a large left atrial volume may need additional treatment, he continued. “So, I think we’ve got a whole lot to learn about ablating persistent atrial fibrillation, and I think there’s value to clinical trials in settling these issues.”
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Wilber DJ. Outcomes of adjunctive left atrial appendage ligation utilizing the Lariat compared to pulmonary vein antral isolation alone: the aMAZE trial. Presented at: AHA 2021. November 14, 2021.
Disclosures
- The aMAZE trial was sponsored and funded by AtriCure.
- Wilber reports receiving research grants from Abbott, AtriCure, and Biosense Webster; receiving honoraria from Biosense Webster; and serving on the executive committee for a Boston Scientific clinical trial.
- Tedrow reports honoraria from Abbott, Boston Scientific, and Baylis Medical; payments for consulting and serving on an advisory board from Biosense Webster; and consulting fees from Thermedical.


Comments