MitraClip Analysis Highlights Questions of Patient Selection in Functional MR
A retrospective study hoped to tease out MitraClip’s impact according to MR etiology, but instead stirs the pot on how to identify patients who’ll benefit.
A new, retrospective study trying to tease out the benefits of MitraClip procedures according to the etiology of mitral regurgitation (MR) hints that, compared with conservative management, interventions (either a clip or surgery) are associated with improved survival in patients with functional MR but not in those with degenerative MR.
Like the many observational studies that preceded the two MitraClip trials that made headlines last year, however, these latest data can only spur discussion and heighten awareness of mitral valve disease, experts say.
In the current study, after a median follow-up of 2.8 years, functional MR patients were more likely to die if treated conservatively than if treated with a MitraClip (Abbott) or surgery. No such signal was seen in the degenerative MR patients, although numbers were low, ruling out comparisons.
According to senior author Jan Van der Heyden, MD, PhD (St. Antonius Hospital, Nieuwegein, the Netherlands), this retrospective analysis was launched prior to the release of the conflicting COAPT and MITRA-FR trial results, yet it shows that baseline characteristics and outcomes in patients treated in daily practice in many ways echo those treated in the positive COAPT trial.
“This is coming from real-life experience,” Van der Heyden told TCTMD. “Before, there was no randomized data so people would say, ‘Well, it's not randomized,’ but now we have randomized data confirming what we see in daily life. That is of great value because the selection we make in our population is not so [strict] as it would be in the patients selected for the randomized trials, because there they selected really the perfect cases amenable for MitraClip therapy.”
Healthier people are going to go to surgery and the slightly less healthy people are going to go to the clip and the people who are really sick are going to get medical therapy. Yogesh Reddy
Commenting on the findings for TCTMD, though, Yogesh Reddy, MD (Mayo Clinic, Rochester, MN), called the results “predictable” and subject to the same concerns faced by similar studies prior to the release of the randomized trials.
“It's very, very difficult to determine any efficacy from this kind of analysis, because the healthier people are going to go to surgery and the slightly less healthy people are going to go to the clip and the people who are really sick are going to get medical therapy,” Reddy said. “No amount of adjustment, statistically, can account for that because there are unmeasured confounders that we can't control for.”
Results of the study were published online recently in EuroIntervention.
Eager for More MR Insights
Van der Heyden and colleagues, including first author Friso Kortlandt, MD (St. Antonius Hospital), looked at survival among 688 high-risk patients with functional MR and 275 patients with degenerative MR, using cox regression and propensity analyses to account for baseline differences between treatment groups. Patients included in the analysis as controls were drawn from the population of patients treated surgically and nonsurgically in the 2 years prior to the MitraClip’s approval in Europe.
In the functional MR group, conservative treatment was associated with higher mortality than were MitraClip procedures (HR 1.79; 95% CI 1.34-2.39), whereas no difference was seen between MitraClip and surgery (HR 0.86, 95% CI 0.54-1.38). The death rate, however, was numerically higher for patients treated with MitraClip rather than with surgery (33% vs 23%), in keeping with the higher mean EuroSCORE II seen in the MitraClip-treated patients versus surgery (8.9 vs 4.7; P < 0.001).
Likewise, Kortlandt and colleagues note in the paper that the surgical cohort had “markedly more favorable characteristics” than did the MitraClip patients. “This is not surprising,” they write, “since surgical therapy for high-risk patients with functional MR was not—and is not—indicated according to European guidelines, whereas MitraClip treatment of such patients may currently be considered.”
Van der Heyden summarized the data by saying: “I think what we’re seeing is the consistency of what's been described before, [namely] that in such patients with HF and mitral valve regurgitation, especially functional regurgitation, they should be treated whether it is surgically or percutaneously. Secondly, what we see in the surgical group is that they are not so high-risk as the patients that are treated with the MitraClip and my conclusion from what we've learned, both from our own center and from the meta-analysis as well, is that we should offer our patients—as we do now—tailored or custom-made therapies, and that can be a surgical or percutaneous approach.”
Just how to identify the patients with functional MR who are best suited to the MitraClip remains a shifting topic—one that has exploded in the wake of the disparate results from COAPT and MITRA-FR.
According to Van der Heyden, he and others who implant the MitraClip device actually met to discuss the two trials’ results following their release and ultimately came up with a “phenotype” of patients based on who was included or excluded from the studies. Ultimately, he said, the patients who appeared to benefit in COAPT and MITRA-FR were similar to those identified in their own retrospective analysis.
“We think that that phenotype of patients is the one that has functional MR and heart failure but is not already in the last phases of heart failure, meaning we should treat our patients even earlier and not wait until they are [NYHA] class IV and have very poor ejection fraction,” he advised.
An “eye-opener” in the current series is that operators typically were not waiting until patients developed severe MR, which in turn exacerbates the ventricular function, Van der Heyden said. “So we didn't wait until we had like 4/4 MR, and I think that's an important message which we also see reported in the COAPT trial [where the proportion of patients with MR 4/4 was 50%] if you compare [it] to the MITRA-FR trial [MR 4/4 = 60%].
But speaking with TCTMD, Reddy stressed that a key fault with Kortlandt et al’s data set is the lack of imaging results. “What is emerging as very important in the randomized trials is how big the left ventricle was and the contribution of the cardiomyopathic process versus the mitral regurgitation into the ventricle,” Reddy noted. “Without echo data, you really can't tease this apart.”
Also missing is critical information on medical therapy—something Van der Heyden also identified as a key shortcoming of his analysis. COAPT, Reddy noted, was very selective in its initial screening, then only randomized 40% of that selected subset. “They were very meticulous in only taking people at maximally tolerated medical therapy,” he said, “because . . . not all patients are going to benefit and we have to study better: what are the parameters that are going to predict who is going to respond and how are we going to select patients?”
Van der Heyden agreed, stressing that importance of optimal medical therapy (OMT) is one idea that must be clearly conveyed to referring physicians. Another is that centers implanting the MitraClip have to have the experience and patient volumes that lead to the best outcomes. As other observers have previously noted, a reduction in MR grade with MitraClip is a key predictor of success with this procedure. In the current study, a MR grade reduction with MitraClip to 2/4 or less was achieved in 93% of patients—that proportion was 91% in MITRA-FR and 95% in COAPT, the authors note.
What Next?
Van der Heyden believes the most important takeaway from this analysis, as well as from the recent MitraClip trials, is that patients with MR should be identified early and referred for heart team review.
“Awareness of the treatments, be it surgery or MitraClip, should be enhanced and highlighted even more because it seems that really a lot of patients with mitral regurgitation are not referred to an interventional center to be treated and that's a very important message,” he said. Despite some of the confusion they may have caused, the two randomized trials have done a great deal to improve awareness of MR diagnosis and referral among cardiologists and in the medical community more broadly, Van der Heyden observed.
His own practice, however, has not changed substantially in the wake of COAPT and MITRA-FR, he noted, adding that his hospital was already a tertiary referral center accustomed to heart team decision-making, with enough patients treated to know that intervening in those with advanced heart failure is likely futile.
“Already we were excluding patients who were in end-stage heart failure, because we could already see that the outcome in these patients was not good so [they were] not benefiting,” Van der Heyden said. “I think other centers will come to the same conclusions, since people are still looking at the MitraClip as new and they are rather skeptical of the [clinical trial] outcomes, so I think physicians will be wise enough not to [treat] those patients who are beyond repair.”
Awareness of the treatments, be it surgery or MitraClip, should be enhanced and highlighted even more because it seems that really a lot of patients with mitral regurgitation are not referred to an interventional center to be treated. Jan Van der Heyden
Reddy, likewise, stressed the need to better hone the patient-selection process. “The next step is really to find out which patients are going to benefit,” he said. Kortlandt et al’s analysis of this hot-button topic “was a real-world experience showing that with these patients, if you carefully select them, their mortality is not terrible. We just have to be careful in saying that the clip is what led them to do better than medical therapy in this kind of analysis.”
Of note, neither COAPT or MITRA-FR included a surgical arm, and the question of whether surgery or MitraClip is preferable in patients with functional MR awaits the MATTERHORN randomized trial. According to Kortlandt and colleagues, MATTERHORN results are expected in late 2019.
There’s also the third eagerly awaited OMT versus MitraClip trial. “What I heard lately is that probably by the end of 2019 we will have more details from RESHAPE-HF 2, with 1-year follow-up,” said Van der Heyden. “People are really hoping there will be a third randomized trial . . . to say something about how we should change the guidelines, because people say we have one positive, one negative trial, and we need a third randomized trial to change the guidelines one way or the other.
Van der Heyden added that his hospital had originally been involved in the RESHAPE-HF 2 study but withdrew when MitraClip therapy “started to boom around the world” and enrollment became so difficult.
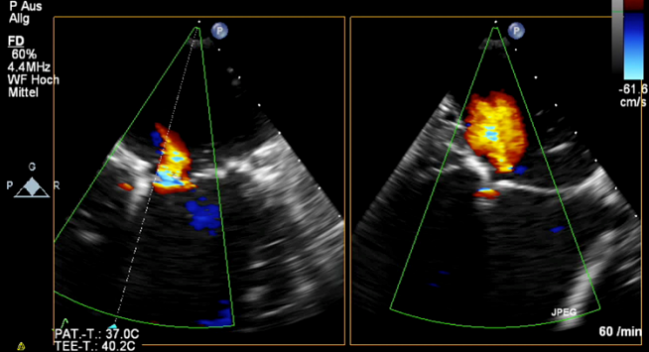
Photo Credit: Baldus S. Two case Presentations: one highly successful and one highly unsuccessful MitraClip in secondary MR. Presented at: TCT 2018. September 23, 2018. San Diego, CA.
Shelley Wood was the Editor-in-Chief of TCTMD and the Editorial Director at the Cardiovascular Research Foundation (CRF) from October 2015…
Read Full BioSources
Kortlandt F, Velu J, Schurer R, et al. Impact of mitral valve treatment choice on mortality, according to etiology. EuroIntervention. 2018;Epub ahead of print.
Disclosures
- Van der Heyden reports research grants from Abbott.
- Reddy reports having no relevant conflicts.


Comments