MitraClip Cuts HF Hospitalizations in Real-World Registry: EXPAND
Understanding predictors of HF hospitalization will hone patient selection and procedure timing, and may improve outcomes.
Heart failure hospitalizations following MitraClip (Abbott) implantation for mitral regurgitation (MR) are markedly reduced, as compared with rates prior to the clip procedure, according to an analysis of the EXPAND registry.
But patients who need to be rehospitalized for heart failure (HF) in the 12 months after their procedures face a markedly lower chance of surviving the first year, which underscores the need to appreciate baseline and procedural factors that increase the risk for post-implant HF hospitalizations, said lead author Mirjam Kessler, MD (University of Ulm, Germany), who presented the EXPAND analysis earlier this week at PCR London Valves 2021.
“I think what we learned from this analysis is that . . . we shouldn't wait too long to do the MitraClip for patients,” she told TCTMD. “So if a patient is stable in New York Heart Association class II, then probably this is the right time to do the MitraClip and not wait until he is in New York Heart Association class IV; we shouldn’t wait until he is highly symptomatic. And I think the same is true for the heart failure hospitalization prior to the MitraClip procedure: we shouldn't wait until the patient is hospitalized.”
Commenting on the results for TCTMD, João Cavalcante, MD (Minneapolis Heart Institute – Abbott Northwestern Hospital, MN), noted that the predictors of subsequent HF hospitalizations identified by Kessler and colleagues speak to the importance of patient selection, particularly for those with functional MR (FMR).
“That's where we need to put our emphasis, focus, and efforts to improve patient selection,” he said, stressing that a clearer picture is emerging of the kinds of patients who will not benefit from clip repair. A key point, he stressed, is that it’s “not just about the valve,” as Kessler et al’s analysis makes clear.
“And it's not just about how symptomatic they are, which is critically important for the decision-making,” said Cavalcante. “You've got to look at the entire context and only when we do that, including the ventricular disease and the extent of that, can we move the needle forward a little bit more and continue to improve. We have therapies that reduce MR—some of them even eliminate it—and yet these patients are progressing in front of our eyes.”
The MitraClip has been available commercially in Europe since 2008 and in the US since 2013, first for the treatment of primary/degenerative MR and later for secondary/FMR. The expanded indication was supported in large part by the results of the COAPT trial. But as Kessler reminded TCTMD, COAPT was a tightly controlled randomized trial requiring rigorous patient selection and optimized heart failure medications.
“In contrast to that, EXPAND is a real-world registry with the conditions, the situations, and the patients we see every day," said Kessler. "I wanted to see how the MitraClip, under these conditions, impacts on heart failure hospitalization.”
EXPANDED Usage
EXPAND is a prospective, observational, single-arm, postmarketing study of MitraClip patients treated at 57 centers in the United States and Europe. The analysis presented by Kessler this week looked at clinical outcomes among patients who required HF hospitalization following transcatheter edge-to-edge repair (TEER) as compared to patients who didn’t, and whether investigators could identify any independent predictors of subsequent hospitalizations.
In all, 1,041 patients participated in the study and the majority (83%) were not hospitalized for HF over the next 12 months, while 181 patients were admitted at least once for worsening HF symptoms.
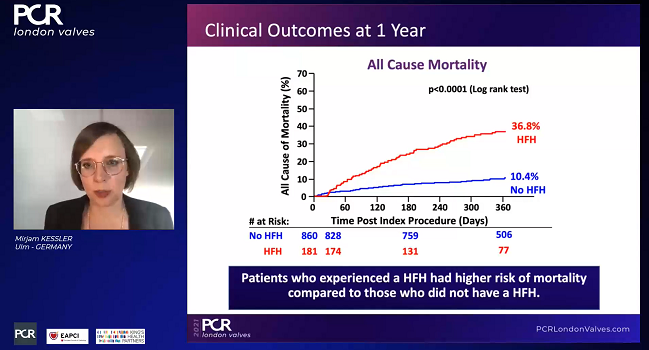
Overall rates of HF hospitalization post-MitraClip were reduced by 63% among EXPAND patients, as compared with rates in the year prior to their procedures (P < 0.001). For those who required hospitalization after TEER, however, all-cause mortality was significantly higher, at 36.8% versus 10.4% (P < 0.0001).
Analyses of MR grade, NYHA classification, and quality of life at 30 days and 1 year showed that improvements in all three endpoints were seen regardless of whether patients required subsequent HF hospitalization. Not surprisingly, however, the magnitude of benefit was attenuated among those requiring hospitalization. For example, by 1 year, 82% of patients in the not-hospitalized group were in NYHA class II or less, whereas that number was just 67.9% in patients who’d required hospitalization (P = 0.003). Likewise, quality of life as measured by the KCCQ score improved to a greater degree from baseline to 1 year among patients who were not hospitalized as compared with those who were, with scores improving by 22 points and 16 points, respectively.
Further analyses identified a range of baseline factors that were independently associated with HF hospitalizations including reduced left ventricular function (≤ 40%), NYHA class III/IV heart failure, prior HF hospitalization, and tricuspid regurgitation of 2+ or greater. Residual MR after MitraClip (≥ 2+) was also a strong predictor of subsequent hospitalization.
Doing Better
Speaking with TCTMD, Cavalcante said he’d also be interested to see EXPAND data on right ventricular function and pulmonary hypertension, which also typically portend worse outcomes in these patients. And he made a “plea” for sites offering the MitraClip to use advanced imaging—functional cardiac CT angiography or cardiac MRI—to get a better handle on the extent of ventricular disease before moving ahead with TEER.
“We need to do a better job because the stakes are high and these are patients’ lives,” he said. “We have to calibrate our expectations and better treat that ventricular disease and better understand that it's not just about the valve, it's about what keeps company with the valvular disease at that stage.”
Kessler and colleagues are also examining background use of HF medications and how this tracked with outcomes but have not yet completed this analysis. She acknowledged that there is a bit of a juggling act that would need to be done between ensuring that medications are optimized before proceeding with TEER, as was done in COAPT, and treating patients sooner in their disease process.
“If this analysis together with COAPT could tell us where the sweet spot is, then we would be really happy, but it's hard to find the sweet spot,” she acknowledged. “If we have a patient who is New York Heart Association class III, and he goes on optimal medication and now is in New York Heart Association class II, then most physicians would probably wait with the MitraClip, [whereas] I think that's the right timepoint to do the MitraClip and our analysis supports that.”
What’s striking, said Cavalcante, is the high mortality rate among patients who needed to be rehospitalized after TEER—nearly 37% for this subset of patients in EXPAND as compared with a 2-year all-cause mortality rate in COAPT of 29%.
“It does make us ponder, are we selecting the right patients?” he said. “I think there's a lot of room from improvement.”
Close collaboration with HF specialists is critical, Cavalcante observed. “Our heart failure colleagues are the ones we have to always lend our ears to, and really work together with them, and I think that can be mutually beneficial.”
It falls to HF specialists to uptitrate the medications that target the ventricular disease, but in some cases, Cavalcante noted, clipping the mitral valve and reducing the MR can allow blood pressure rates to come up, allowing medication dosages to be increased.
Shelley Wood was the Editor-in-Chief of TCTMD and the Editorial Director at the Cardiovascular Research Foundation (CRF) from October 2015…
Read Full BioSources
Kessler M, Rottbauer W, Stephan R, et al. Predictors of heart failure hospitalization and its impact on clinical outcomes. Results from the contemporary MitraClip EXPAND study. Presented at: PCR London Valves 2021. November 21, 2021.
Disclosures
- Kessler reports having no conflicts.
- Cavalcante reports consulting for Boston Scientific, Abbott Structural, Edwards Lifesciences, Medtronic, VDyne, TriFlo, and WL Gore.





Comments