MitraClip Viable in MI Patients With Acute MR, Including Patients in Shock: IREMMI
All patients were turned down for surgery and medical therapy is known to be largely ineffective for these high-risk patients.
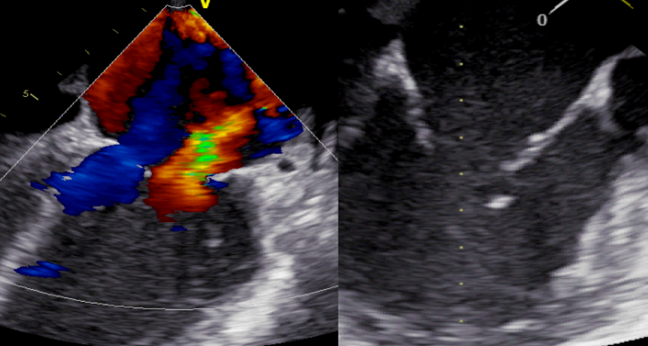
For patients with acute mitral regurgitation (MR) following myocardial infarction, including those who present with and without cardiogenic shock, treatment with MitraClip (Abbott) may be a viable option for this high-risk cohort who have no surgical alternative, according to a small, retrospective series.
Overall, investigators reported that percutaneous repair was associated with “acceptable rates of death and rehospitalization,” including in those with acute MR who presented in cardiogenic shock, as well as improvements in MR grade and NYHA functional class.
After a median follow-up of 7 months, 16.3% of patients with acute MR and cardiogenic shock following MI died after treatment with MitraClip compared with 9.3% of patients who didn’t develop cardiogenic shock (P = 0.377). The combined rate of death or rehospitalization due to heart failure was 28% and 25.6% in the patients with acute MR with and without cardiogenic shock after MI (P =0.793).
Presenting the IREMMI results during today’s late-breaking clinical science session at TCT Connect 2020, Rodrigo Estévez-Loureiro, MD, PhD (University Hospital Alvaro Cunqueiro, Vigo, Spain), explained that MR stemming from papillary muscle rupture was infrequent in their series, with most of it due to acute ventricular remodeling and restriction of the posterior mitral leaflet.
Mortality for patients with severe MR after MI is extremely high, he said.
“Until recently, surgery was the only alternative, but there have been some reports of MitraClip being used in this scenario,” said Estévez-Loureiro. However, all patients in the present study had been turned down by the surgical team, leaving medical therapy the only option. “We know medical therapy is associated with the highest rate of mortality—50% at 30 days,” for these patients, he said.
IREMMI Registry
In this registry, investigators included consecutive patients with acute MR complicating MI treated with MitraClip at 18 centers in Europe, North America, and Israel between 2016 and 2020. Over 4 years, the group enrolled just 93 patients, including 50 who presented in cardiogenic shock and 43 without shock. For those in cardiogenic shock, MitraClip to treat acute MR was implanted 24 days after presenting to hospital for MI. For those not in cardiogenic shock at presentation, MitraClip was implanted 33 days after the MI.
At baseline, 86% and 79% of shock and nonshock patients had MR grade 4. Immediately after MitraClip implantation, the majority of patients had a significant improvement in MR grade, with more than 60% getting to an MR grade of 0-1. These benefits were observed in shock and nonshock patients. At 3 months, the results were similar, with again no difference in MR improvement seen between shock and nonshock patients treated with MitraClip. NYHA functional class was also improved: while the majority were in NYHA class IV at baseline, 80% and 85% of the cardiogenic shock and noncardiogenic shock patients, respectively, were in NYHA class I or II at follow-up (P = 0.608 for difference between groups).
With respect to clinical events, Estévez-Loureiro said cardiogenic shock was not associated with an increased risk of mortality or hospitalization for heart failure.
“The only variable that was significantly associated with this composite endpoint was procedural success,” he said. As such, cardiogenic shock, if its adequately supported, doesn’t influence short- and mid-term outcomes of percutaneous repair with MitraClip and shouldn’t preclude its use, said Estévez-Loureiro.
Dee Dee Wang, MD (Henry Ford Health System, Detroit, MI), who spoke during a media briefing where the results were announced, praised the investigators for the study, noting that it’s challenging to collect data on patients at such high risk. She questioned why there was a long delay between MI presentation and treatment of acute MR. In response, Estévez-Loureiro said the strategy of most centers had been to cool down the cardiogenic shock patient and then provide mechanical support and medical therapy before considering percutaneous repair with MitraClip.
“In the end, after two or three failed therapies, then it becomes an option,” he said. For the cardiogenic shock patient, he also stressed stabilization is critical.
Cardiac surgeon Michael Borger, MD, PhD (Leipzig Heart Center, Germany), who moderated the late-breaking science session, said that when compared to ACS patients with acute MR sent for surgery, the mortality rate in the IREMMI series “is very, very respectable.” Estévez-Loureiro said researchers are currently collecting and analyzing outcomes of patients with severe MR following MI treated with medical therapy and surgery to serve as control arms for comparisons with MitraClip.
“I don’t want to unveil our results, but they’re quite interesting, and hopefully we’ll be releasing them in a few months,” said Estévez-Loureiro.
Panelist Jeroen Bax, MD (Leiden University Medical Center, the Netherlands), attributed the solid IREMMI outcomes to the expertise of the hospitals and physicians participating in the registry. He questioned whether the geometry of the ventricle had an impact on the efficacy of the MitraClip to treat the mitral valve. LV dimensions, relative to MR severity, have dominated discussions about the MitraClip’s efficacy in clinical trials to date. Estévez-Loureiro said that geometry was not a factor.
“All these procedures were done in highly experienced centers, so people were quite used to treating complex anatomies,” he said. With the mechanism underlying MR being LV remodeling and restriction of the posterior leaflet, this might make it a little bit easier for MitraClip implantation. Nonetheless, even in the few patients with papillary muscle rupture, operators were also successful implanting the device, Bax noted.
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Estévez-Loureiro R, on behalf of the IREMMI investigators. Outcomes of MitraClip in patients with acute mitral regurgitation in acute MI with and without cardiogenic shock: IREMMI. Presented at: TCT 2020. October 17, 2020.
Disclosures
- Estévez-Loureiro reports grant/research support from Abbott Vascular and consulting fee/honoraria from Abbott Vascular and Boston Scientific.
- Wang reports research support from Boston Scientific and consulting fees/honoraria from Edwards Lifesciences, Boston Scientific, and Synchrony Labs.
- Borger reports consulting fees/honoraria from Edwards Lifesciences, Medtronic, Abbot Vascular, and CryoLife.
- Bax reports no relevant conflicts of interest.


Comments