New NACMI COVID-19 Numbers Highlight Quality Care, Sobering Reality
Now with nearly 1,000 patients, the registry shows that primary PCI is still dominant and linked to better outcomes.
Results from the North American COVID-19 Myocardial Infarction (NACMI) registry continue to confirm that STEMI care hasn’t suffered during the pandemic, with the majority of patients undergoing prompt primary PCI.
Yet patients who have diagnosed COVID-19 on top of STEMI do see sharply higher mortality compared with typical patients, investigator Payam Dehghani, MD (Prairie Vascular Research, Regina, Canada), pointed out at a press conference ahead of the Society for Cardiovascular Angiography and Interventions (SCAI) 2021 meeting.
“One in three does not make it out,” he observed. That said, “primary PCI is common, it’s feasible, and it’s associated with reduced mortality. And this is in keeping with our current guidelines.”
NACMI is a joint effort by SCAI, the Canadian Association of Interventional Cardiology, and the American College of Cardiology Interventional Council. The registry was launched early in the pandemic in order to track the impact of multiple factors, among them the apparent drop in acute MI cases coming to the hospital, any added morbidity and mortality contributed by the virus, as well as a potential shift to lytics as a management strategy, which was an idea floated early on in the pandemic to help hospitals hard hit with COVID-19 patients.
The latest analysis, presented today by Dehghani, spans more than 975 patients known or expected to have COVID-19. It comes on the heels of a peer-reviewed paper, recently published in the Journal of the American College of Cardiology, that explores sociodemographic patterns and outcomes among 698 patients, up from just 594 in the NACMI registry’s first report last fall.
“We are still recruiting, and we are still wanting other sites to reach out to us,” Dehghani told his virtual SCAI audience. “There are still many questions to be answered.”
Comorbidities, Race/Ethnicity Differ
Dehghani’s presentation included 331 patients with confirmed COVID-19 and 645 who tested negative after being suspected of having COVID-19, classified as persons under investigation (PUI). All had either ST-segment elevation or new-onset left bundle branch block on 12-lead ECG, as well as clinical signs of ischemia. There were no exclusion criteria.
COVID-positive patients were more likely to present with dyspnea compared to PUI (51% vs 35%) and more apt to have in-hospital presentation of STEMI (7% vs 2%). On the other hand, they were less likely than PUI to have chest pain (53% vs 80%). On chest X-ray, the COVID-19 group had a higher prevalence of infiltrates (45% vs 16%). Two patient characteristics also stood out: the COVID-19 patients were much more likely than PUI to be non-Caucasian (55% vs 25%), and they also had a higher prevalence of diabetes (44% vs 33%). All of the above comparisons were statistically significant (P < 0.001).
“About one in five of the COVID-positive patients did not receive an angiogram,” Dehghani noted in his presentation. For 22% of them, the reason was unknown. The choice to pursue conservative management was the most common explanation, for 38%. Other factors were pericarditis/myocarditis, Takotsubo cardiomyopathy, and COVID-related severe respiratory illness.
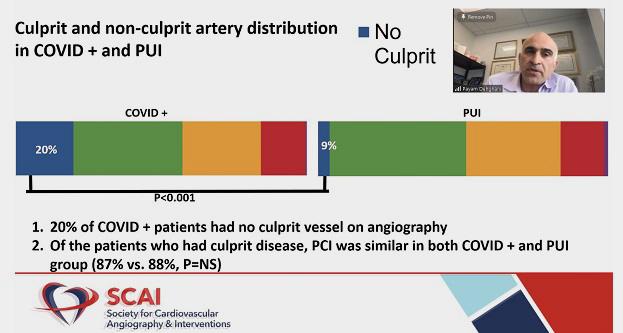
For the subset of patients who did undergo angiography, thrombolytic use was less than 3% in the COVID-19 group. By far, most patients had primary PCI. Medical therapy was more common in the COVID-19 group than in PUI (23% vs 13%; P < 0.001). Fully 20% of the COVID-19 patients were found to have no culprit vessel on angiography.
In further analyses, the COVID-19-positive and PUI groups were also compared to age- and sex-matched controls from the Midwest STEMI Consortium who had been treated before the onset of the pandemic (January 2015 to December 2019). Here, in-hospital outcomes differed considerably between the COVID-19 patients versus both the PUI and the controls, with significant differences in the primary endpoint (in-hospital death, stroke, recurrent myocardial infarction, or repeat unplanned revascularization), as well as mortality, reinfarction, and lengths of stay in the ICU and in the hospital.
NACMI Registry: Updated Clinical Outcomes
|
|
COVID-19 |
PUI |
Controls |
|
Primary Endpoint |
35% |
14%* |
5%* |
|
Mortality |
33% |
11%* |
4%* |
|
Stroke |
3% |
2% |
– |
|
Reinfarction |
2% |
1%* |
– |
|
Median ICU Stay, days |
3 |
2* |
– |
|
Median Total Stay, days |
6 |
3* |
2* |
* P < 0.001 vs COVID-19 group
Independent predictors of death among COVID-19 patients included intubation, cardiogenic shock pre-PCI, in-hospital STEMI presentation, diabetes, and older age. Primary PCI, on the other hand, significantly improved the odds of survival.
Much Left to Learn
Sripal Bangalore, MD (NYU Langone Medical Center, New York, NY), commenting on the results for TCTMD, said, “My first reaction to this is, when we published data from New York in the very early part of the pandemic, the mortality was like 50% and at that point, we’d hoped that with more patients and more experience, the mortality would come down.”
As such, he said, it’s “sobering that even now with so many patients, the mortality rate for the COVID STEMI is 33%. I mean, that’s very, very high,” approaching what’s seen with cardiogenic shock. It’s possible, Bangalore acknowledged, that more deaths were concentrated in the early waves and that mortality has decreased over time, averaging out to the snapshot provided here.
Asked by TCTMD if or when NACMI investigators plan to track any shifts over the course of the pandemic, Dehghani said that the registry’s design has made that tricky. In order to waive informed consent, there had to be no identifiers. “Part of not having an identifier is not having a date of an MI, but we have asked for an amendment to at least be able to capture [data] quarterly to look to see if there’s been a trend in improvement of care as we’ve gotten better in dealing with this pandemic,” he said, adding that the analysis is in the planning stages. The group is also working to create ECG and angiographic core labs.
Kirk Garratt, MD (ChristianaCare, Newark, DE), at the media briefing, queried whether it was possible to tease out how much STEMI itself contributed to the mortality rate among COVID-19 patients.
“It turns out to be very difficult to actually determine the cause of death in this patient population,” Dehghani said. Autopsy data for COVID-19 patients more generally, not just those with STEMI, show that around 40% have microthrombi in their coronary arteries, Dehghani noted, and it’s possible that pulmonary involvement also played a role alongside STEMI.
Santiago Garcia, MD (Minneapolis Heart Institute Foundation, MN), lead author of the recent JACC report from NACMI, told TCTMD earlier this month that the registry is well equipped to address the evolving picture of STEMI care and outcomes in COVID-19 because there will be prospective follow-up of discharged patients up to 1 year. In addition to expanding sites in Canada, “we’re also trying to understand if these new variants that are more contagious and supposedly more lethal have an impact” on which patients are coming to the cath lab, Garcia said.
Bangalore pointed out that the actual practice of performing primary PCI in the COVID-19 setting is a “completely different ball game” compared with typical STEMI cases.
“It’s vastly different. We were really surprised by the amount of thrombus we see in these patients,” he said. While there is a spectrum of severity, for the most-challenging COVID-19 STEMIs, “we have tried all the techniques in the books” from thrombus aspiration to coronary lytics and laser, said Bangalore. Discussion continues on how to best handle the heavy thrombus burden.
Caitlin E. Cox is Executive Editor of TCTMD and Associate Director, Editorial Content at the Cardiovascular Research Foundation. She produces the…
Read Full BioSources
Dehghani P. Update on the North American COVID-19 Myocardial Infarction (NACMI) registry. Presented at: SCAI 2021. April 28, 2021.
Disclosures
- Dehghani and Bangalore report no relevant conflicts of interest.
- Garcia has received institutional research grants from Edwards Lifesciences, Boston Scientific, Medtronic, and Abbott Vascular; has served as a consultant for Medtronic and Boston Scientific; and has served as a proctor for Edwards Lifesciences.





Comments