Newest Resorbable Magnesium Scaffold Shows Promise in BIOMAG-1
Serial OCT data presented this week at EAS 2023 suggest the vessel shows signs of stabilization, says Hector Garcia-Garcia.
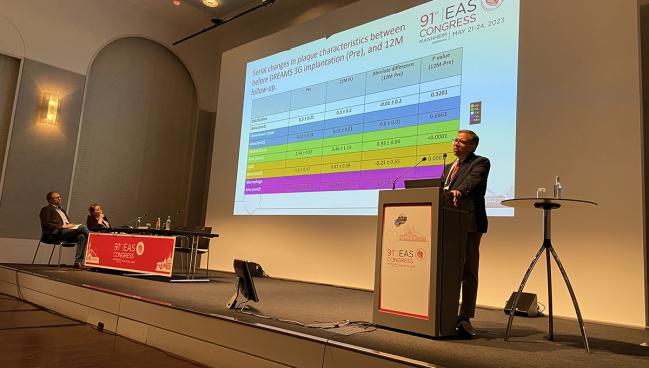
MANNHEIM, Germany, and PARIS, France—Serial coronary imaging of patients implanted with a resorbable magnesium scaffold (Dreams 3G; Biotronik) for coronary artery disease suggests “favorable healing” of the vessel wall based on changes in plaque composition, according to results of the small BIOMAG-1 study presented this week at the European Atherosclerosis Society (EAS) Congress 2023.
On optical coherence tomography, investigators observed a significant reduction in the total lipid area, as well as a significant increase in the amount of fibrous tissue, in this first-in-human study with the newest-generation bioresorbable scaffold.
“It seems to make the vessel wall heal in a very benign way,” Hector M. Garcia-Garcia, MD, PhD (Georgetown University/MedStar Washington Hospital Center, DC), who presented the results at the EAS Congress, told TCTMD. “You’re increasing fibrotic tissue, which is the tissue that helps stabilize the plaque, helps seal it from a potential rupture. On the other hand, you have this decrease in lipids, the bad guy in the vessel wall. These two combined effects make us think of plaque stabilization with the device.”
The sirolimus-eluting scaffold is made from a proprietary magnesium alloy and has been on the European market for many years in a different form. However, it’s been recently redesigned to decrease the strut thickness while also increasing the amount of radial force, but resorbing completely by 1 year. Depending on the diameter of the scaffold, strut thickness ranges from as low as 99 up to 147 μg with the larger scaffolds. The prior iteration of the scaffold, which was known commercially as Magmaris and had a strut thickness of 150 μg, disappointed in that the amount of late lumen loss was not comparable with contemporary drug-eluting stents. Imaging studies showed that earlier device was associated with neointimal hyperplasia and constrictive remodeling.
Even this latest version of the scaffold is “quite an old device—this is maybe the third iteration—but it’s the one that will be used in randomized, clinical trials, which have been announced and are expected to be launched at the end of the year,” said Garcia-Garcia.
OCT Suggests Plaque Stabilization
BIOMAG-1 included 116 patients (mean age 61 years; 77.8% male) with stable or unstable angina, documented silent ischemia, or hemodynamically stable NSTEMI. The majority of lesions were classified as type B2/C and just 2.6% were considered moderately or severely calcified.
Just a week prior to the EAS presentation, the BIOMAG-1 investigators, led by Michael Haude, MD, PhD (Rheinland Klinikum Neuss GmbH, Neuss, Germany), presented 12-month angiographic and clinical data at EuroPCR 2023 in Paris, France. In-scaffold late-lumen loss (LLL), the study’s primary endpoint, was 0.24 mm at 12 months, which is on par with modern-day DES and significantly lower than the 0.39 mm seen in BIOSOLVE-II with the second-generation Magmaris device. In-segment LLL was 0.10 mm with Dreams 3G compared with 0.25 mm with the second-generation scaffold.
On OCT, Haude said the scaffold struts were “no longer discernible” at 12 months, although remnants could be seen on IVUS.
Clinically, the rate of target-lesion failure was 2.6%, which was the result of three clinically driven target-lesion revascularizations. There were no deaths, MI, or probable/definite scaffold thromboses.
Upendra Kaul, MD (Batra Heart Center, New Delhi, India), one of the discussants during the EuroPCR hotline session, agreed the third-generation scaffold is an upgrade over the earlier versions, noting, “We’re seas apart from the first magnesium [scaffold] that used to dissolve under your eyes.” The strut thickness is reduced across all stent diameters, all without a loss of radial strength. He also praised the lower rate of LLL compared with what came before.
“Having said this, this is just the beginning,” said Kaul. BIOMAG-1 included relatively simple patients undergoing PCI, he noted, and a randomized trial against a “very good drug-eluting stent” is a must.
Better Long-term Outcomes? Hopefully
At the EAS Congress, Garcia-Garcia presented mechanistic data based on serial OCT imaging taken before scaffold implantation and at 6 and 12 months. The goal, he said, was to determine if there were any specific plaque types that might respond better to the implanted scaffold. “It’s fully resorbed over 12 months, and we wanted to understand the interplay between the tissue components where the scaffold lands versus the actual effects of the device on the vessel wall,” he said.
On angiography, as noted, the mean in-scaffold LLL was 0.24 mm at 12 months. When investigators stratified patients into terciles based on the amount of lumen loss—tercile 1, 2, and 3 with LLL < 0.09 mm, 0.09-0.27 mm, and > 0.27 mm, respectively—they found that those with the least amount of LLL had significantly less fibrotic tissue. They also performed the same analysis using OCT, which has better resolution for the various plaque components. Here, they found similar outcomes: patients with the least amount of lumen loss from the time of PCI to 12 months were those with less fibrotic tissue.
“The larger the amount of fibrotic tissue present at the time of the treatment, the more likely the patient is to experience luminal loss over time,” said Garcia-Garcia. “When the scaffold is implanted in a very fibrotic lesion, it’s like a rubber band. You deploy the device, it temporarily opens up the vessel, but the band comes back in once the scaffold disappears over time.”
He speculated that this might have clinical or research implications, noting that it’s possible an ideal candidate for the scaffold could be patients with less fibrous tissue.
With respect to serial changes in the overall plaque composition from pre-PCI to 12 months, Garcia-Garcia highlighted the increase in the amount of fibrotic tissue (2.54 to 3.46 mm2) as well as corresponding decline in lipid content (1.1 to 0.87 mm2), findings suggestive of plaque stabilization. In general, the bioresorbable-scaffold field has lost some of its luster in light of the high-profile collapse of Abbott’s original Absorb device. To TCTMD, Garcia-Garcia said the positive changes seen on OCT will hopefully translate into significantly reduced risk of long-term stent-related adverse events seen with other bioresorbable scaffolds, such as Abbott’s.
The BIOMAG-II study, which is also being led by Haude, is expected to launch sometime later this year. Investigators plan to enroll roughly 1,700 patients and randomize them to PCI with the resorbable magnesium scaffold or the Xience DES (Abbott). Follow-up is planned for 5 years with BIOMAG-1, but it’ll be clinical follow-up only, said Haude, as it was challenging enough to have the patients agree to serial invasive imaging at 6 and 12 months.
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Haude M, et al. A new resorbable magnesium scaffold for de novo coronary lesions, the DREAMS 3G: one-year results of the BIOMAG-1 first-in-human study. Presented at: EuroPCR 2023. May 17, 2023. Paris, France.
Garcia-Garcia HM, et al. Temporal changes in coronary plaque as assessed by an artificial intelligence-based optical coherence tomography. Presented at: EAS 2023. May 22, 2023. Mannheim, Germany.
Disclosures
- Haude reports serving as a proctor for Cardiac Dimensions, receiving grants/research support from Biotronik, and receiving honoraria/consulting fees from Biotronik, OrbusNeich P&F, and Shockwave Medical.





Comments