Next-Gen MitraClip Performs as Well as Earlier Device in COAPT: EXPAND
At 1 year, a benefit was seen in those who received the NTR and XTR devices, as well as those with small and large EROAs.
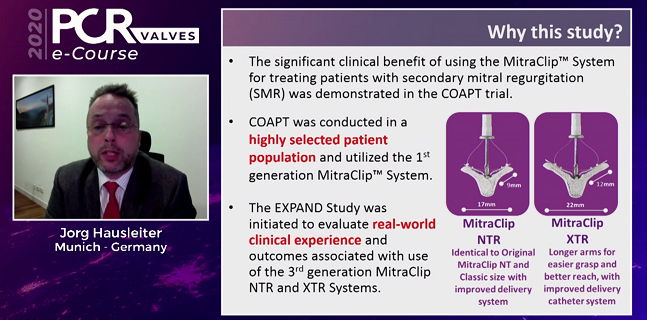
One-year mortality rates for patients with secondary mitral regurgitation (MR) treated with the next-generation MitraClip NTR and XTR systems (Abbott) as part of the real-world, global EXPAND registry compare favorably with outcomes seen in the landmark COAPT trial, according to an analysis presented this week.
The mortality rate for secondary MR patients treated with either MitraClip NTR or XTR was 17.7%, which is slightly lower than the 19.1% mortality rate observed at 12 months in COAPT. The rate of hospitalizations for heart failure in the EXPAND registry was 26.0%, which was a shade higher than the rate seen in COAPT.
“COAPT is a very nice and important clinical trial, but the patient population was highly selected,” lead investigator Jörg Hausleiter, MD (Ludwig-Maximilians-Universität, München, Germany), told TCTMD. “In EXPAND, this was a real-world study, and we included patients as we see them today where we think the MitraClip is going to be beneficial. There aren’t the same constraints as we have in a randomized trial in terms of inclusion/exclusion criteria. This is real-world, representing daily practice.”
The EXPAND study was conducted across 57 centers in the United States and Europe. Presenting the results during the virtual PCR Valves e-Course 2020, Hausleiter reminded the audience that the use of percutaneous MitraClip in patients with heart failure and severe functional MR in COAPT significantly reduced not only the primary endpoint of heart failure rehospitalizations, but also mortality at 2 years. Those results contrasted with MITRA-FR, which also tested MitraClip in secondary MR but didn’t show a reduction in all-cause mortality or heart failure hospitalizations.
In October at TCT Connect 2020, Saibal Kar, MD (University of California, Los Angeles), presented data from EXPAND on 722 patients with primary (degenerative) and secondary (functional) MR treated with the next-generation MitraClip. This newest EXPAND analysis focuses on a range of patients with secondary MR and provides a more direct comparison with clinical outcomes in COAPT.
From COAPT to the Real World
In total, there were 413 patients in the registry with secondary MR treated with the next-generation MitraClip NTR (44%) or XTR (56%) devices, which are newer iterations of the first-generation device used in COAPT. In total, 370 patients completed 30-day follow-up and 285 patients had complete clinical and echocardiographic follow-up at 1 year.
With respect to functional improvement, more than 90% of patients had MR grade ≤ 1+ through 1 year while 99.6% of all treated patients had MR ≤ 2+. In contrast, 94.5% of patients treated with MitraClip in COAPT had MR ≤ 2+ at 1 year, said Hausleiter. “This MR reduction translated into a significant improvement in the New York Heart Association class and quality of life,” he said.
In a comparison with the COAPT patients, Hausleiter said the two groups were well matched, although the effective regurgitant orifice area (EROA) was smaller in EXPAND patients (0.30 vs 0.41 cm2), suggesting the real-world registry patients had relatively less-severe MR. Additionally, the LV end-diastolic volume index was smaller in the EXPAND patients than in COAPT (97.9 vs 101.0 mL/m2) and LVEF was higher (39.4% vs 31.3%).
When stratified by baseline EROA, there were no significant differences in mortality or HF hospitalizations at 1 year, nor were there any differences in symptomatic improvement or changes in functional status.
To TCTMD, Hausleiter said there has been a large debate as to why COAPT and MITRA-FR differed. One hypothesis is that COAPT investigators treated patients with relatively more-severe MR and smaller LVs than the French trial, suggesting the MITRA-FR patients were more advanced in terms of heart failure. “The EXPAND registry fits right between the two trials,” he said. “Now we’re treating patients with smaller ventricles who are probably in an earlier stage of their heart failure process.”
Additionally, some speculated that COAPT was positive because the MR was so significant. In the registry, physicians are still treating patients with severe MR, although not as severe as in COAPT given the differences in EROA. But the new analysis shows that these patients obtain the same clinical benefit from the MitraClip. “It’s an expansion in terms of MR severity to patients with less, but still severe MR, and to patients with ventricles that aren’t too dilated,” said Hausleiter.
These results, he added, indicate that “this procedure should not be withheld from symptomatic secondary MR patients based on the EROA value.” For patients with secondary MR who are repeatedly hospitalized for HF, the EROA value can be misleading clinically, he said during his Hot Line presentation. MitraClip was also reported to be effective in patients with EROAs < 0.3 cm2 and ≥ 0.3 cm2 in the EuroSMR Registry, he noted.
“So, very consistent results across different studies,” said Hausleiter. Overall, the improvements in symptoms and quality of life are encouraging in this expanded patient population given the symptomatic burden of secondary MR, he added.
No Difference in Clips
Nicola Piazza, MD, PhD (McGill University Health Center, Montreal, Canada), one of the discussants following Hausleiter’s presentation, asked whether there were any differences in outcomes among MR subtypes, such as ischemic versus nonischemic MR, and Hausleiter said no such differences were observed. In terms of safety, Nicolas Dumonteil, MD (Clinique Pasteur, Toulouse, France), questioned how well the devices performed, since there have been reports of leaflet tears and single leaflet device attachment requiring surgical intervention.
Hausleiter said there was a separate clinical event committee in EXPAND to adjudicate outcomes and safety, noting that single leaflet device attachment and leaflet injuries were observed in approximately 2.2% of patients in EXPAND compared with 0.7% in the COAPT trial. The researchers also observed no significant difference in adverse events among patients who received the NTR or XTR devices. The XTR has longer clip arms and is designed to facilitate better leaflet capture, whereas the NTR is the same size as the original MitraClip but has an improved delivery system.
To TCTMD, Hausleiter said that with the longer clip arms, there was some initial worry the XTR device would lead to more leaflet injury because it grabs more tissue, which exerts greater tension on the leaflet and can lead to rupture or tearing. This has been observed outside the EXPAND registry, and while there were numerically more leaflet adverse events with XTR in the registry, the difference was minimal compared with NTR and wasn’t statistically significant.
“We were not able to show that one device had more complications than the other, which I think is important to realize,” he said. “On the other hand, we also had a lot of enthusiasm initially for the XTR but the NTR is a very good device which can be used in many situations. This study has not shown that one device is better in terms of outcomes or has more complications. Both are very, very safe.”
Piazza pointed out there is limited long-term data on use of MitraClip in secondary MR, noting the ACCESS-EU postapproval study was limited to just 1 year. Hausleiter said the global EXPAND Registry with the NTR and XTR devices is limited to 1 year given that there is already a new iteration of MitraClip that has received CE Mark approval in Europe. Another registry is planned, this one for patients implanted with the MitraClip G4 device, and that study is scheduled for 5-year follow-up.
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Hausleiter J, on behalf of the global EXPAND investigators. Contemporary, real-world clinical outcomes with the next-generation MitraClip (NTR/XTR) system in patients with secondary mitral regurgitation: results from the global EXPAND Registry. Presented at: PCR Valves 2020. November 23, 2020.
Disclosures
- Hausleiter reports honoraria and research support from Abbott Vascular and Edwards Lifesciences.


Comments