No-Implant Shunt for HF Looks Safe, Feasible in Early Snapshot
There are still a lot of unknowns, including how best to excise the tissue and whether the shunt will improve patient outcomes.
Captured from: Vardi GM. InterShunt: the EASE-HF results. Presented at: TVT 2023. June 8, 2023. Phoenix, AZ.
PHOENIX, AZ—A no-implant interatrial shunt (PAS-C; InterShunt Technologies) delivered percutaneously appears to reduce pulmonary capillary wedge pressure (PCWPs) and provide symptomatic relief for patients with heart failure with preserved ejection fraction (HFpEF), according to the results of EASE-HF.
The study was very small with just 10 patients, but Gil Vardi, MD (St. Louis Heart & Vascular, MO), who presented the results last week at TVT 2023, said postprocedure left-to-right atrial flow was observed in all patients and that there were no adverse events or complications observed. Vardi, who founded the company developing this shunt technology, said EASE-HF “demonstrates the safety and feasibility” of the procedure, noting the atrial shunt remained durable out to 6 months.
In a second presentation, Christopher Meduri, MD (Karolinska University Hospital, Stockholm, Sweden), provided an update on another no-implant shunt (Alleviant), one that is also being tested in patients with HF with midrange EF (HFmrEF).
Across four study programs, 38 patients have been treated so far, with the device safely and successfully establishing a shunt between the left and right atrium. In follow-up of 33 patients at 12 months, investigators observed improvements in NT-proBNP, functional capacity, and quality-of-life metrics. Additionally, peak exercise PCWP also declined in the shunted patients.
Interatrial shunts are designed to reduce left atrial pressure and volume overload, particularly in patients with HFpEF, although they are also being tested in those with HFmrEF or heart failure with reduced EF (HFrEF). In the REDUCE LAP-HF II trial, which is the only randomized, sham-controlled study to date, an atrial shunt didn’t reduce HF events or improve health status in more than 600 patients with HFpEF. There was a signal of benefit in some subgroups, such as those without latent pulmonary vascular disease and those without pacemakers, which encouraged investigators.
As reported by TCTMD, excitement persists for the technology, partly on the basis of other single-arm studies showing that shunt creation can improve exercise capacity and quality of life, as well as reduce PCWP at rest or during exercise. But it’s very early days.
In the EASE-HF study, peak PCWP declined from 32.4 mm Hg at baseline to 26.7 mm Hg at 30 days. At 6 months, all 10 patients had NYHA class II symptoms and there was a significant increase in 6-minute walk test distance, said Vardi. Quality of life also improved, with nine of 10 patients having a more than 15-point improvement in the Kansas City Cardiomyopathy Questionnaire score. NT-proBNP levels also significantly declined from baseline to 6 months.
With the Alleviant shunt, Meduri said investigators are currently embarking on an ambitious study, with anywhere from 400 to 700 patients expected to be enrolled in the ALLAY-HF trial led by James Udelson, MD (Tufts Medical Center, Boston, MA). That trial will include patients with symptomatic HFpEF or HFmrEF, which includes those with LVEF ≥ 40%.
Leaving Nothing but a Hole
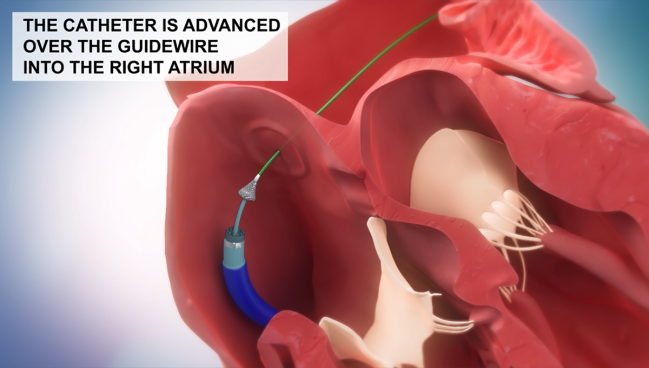
Unlike other atrial shunts being tested, the PAS-C and Alleviant technologies (as well as a third, NoYa) leave no permanent implant as scaffold. Instead, PAS-C uses a mechanical cutting approach, first capturing and then excising tissue from the interatrial septum. The Alleviant shunt differs from PAS-C in that it uses radiofrequency (RF) energy to create the shunt.
To TCTMD, Meduri said the rationale for the no-implant approach is to avoid leaving something behind that might interfere with future left-sided procedures.
“The ability to navigate the septal space to do another intervention on the left side, if you have a device in the septum, is significantly more challenging,” said Meduri. “It doesn’t make it impossible, but it does make it harder to get over, and when it’s harder you might not get an optimal transseptal puncture.” As a result, it may be more difficult to achieve the best possible result for these left-sided procedures.
Even on its simplest level, “leaving behind something in the body leaves the patient at risk for something going wrong,” said Meduri. “The ability to provide the same result with nothing left in the body is the optimal way. Most people, conceptually, can understand that pretty well.”
There’s also the possibility that leaving no rigid supporting structures against the septum might also be beneficial for hemodynamics.
During the TVT session, Samir Kapadia, MD (Cleveland Clinic, OH), one of the panel discussants, questioned what happens afterwards with no-implant shunts, noting that one of the concerns is that after the removal of the tissue, depending on the anatomy of the septum, the hole might either shrink, or worse, continue to enlarge. “This is an issue,” Kapadia said. “Sometimes, when you create a hole, it can get bigger, especially with a flimsier septum.”
Continuing follow-up in EASE-HF may help answer this question. According to Vardi, patients are being followed for 1 year, which will also give investigators an opportunity to look for any changes in the shunt’s dimensions.
Meduri said there are animal data testing different approaches to creating a patent, implant-free shunt. With the RF approach, the tissue at the shunt’s edges is almost sealed after healing, the goal being to keep the shunt’s size consistent, he said, rather than shrinking over time.
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Vardi GM. InterShunt: the EASE-HF results. Presented at: TVT 2023. June 8, 2023. Phoenix, AZ.
Meduri C. Alleviant Medical: no-implant interatrial shunt for chronic heart failure. Presented at: TVT 2023. June 8, 2023. Phoenix, AZ.
Disclosures
- Vardi is the chief medical officer of InterShunt Technologies.
- Meduri reports consulting fees/honoraria from Boston Scientific, Alleviant Medical, Cardiovalve, Abbott, and Vdyne. He is a nonemployed chief medical officer of Anteris and has stock options in Alleviant Medical, XDot, and V2V.





Comments