OCT and MRI Find an MI Cause in 85% of Women With MINOCA: HARP
The findings support a role for OCT on top of CMR, already urged by guidelines. How outcomes might change remains unclear.
Multimodal imaging in women presenting with myocardial infarction with nonobstructive coronary arteries (MINOCA) on angiography identified a mechanism of injury in nearly 85% of women participating in the HARP study. That number is a striking figure for a condition that disproportionately affects women and, for decades, saw them being sent home from hospital emergency rooms with “false-positives” and no concrete diagnosis.
A number of recent guidelines already recommend additional imaging when MINOCA is diagnosed on the basis of telltale symptoms and a troponin rise, even if no obstructions are found. HARP, demonstrating that cardiac MRI (CMR) and optical coherence tomography (OCT) provide additive and complementary information, adds heft to those recommendations, said lead investigator Harmony R. Reynolds, MD (NYU Grossman School of Medicine, New York, NY).
“Naturally I think it’s a big deal,” Reynolds told TCTMD. “It’s my study. But I think it is very helpful for patients to know what’s wrong with them, and I've encountered many women who come for an additional opinion having been told the doctor was not sure if there was a heart attack or not, or was not sure how to treat it. And that generates a substantial amount of anxiety in people when a doctor says, ‘I'm not sure what's wrong with you.’ Being able to give a more specific diagnosis to 85% of women with heart attack and open arteries will be very powerful in their care.”
Others echoed that view during the main-event presentation. “Kudos to you,” session co-moderator Roxana Mehran, MD (Icahn School of Medicine at Mount Sinai, New York, NY), told Reynolds. “Finally we can say that this is not just crazy women. There is really something going on. . . . Making that diagnosis is going to be incredibly important.”
Reynolds presented the results as a late-breaking clinical trial during the virtual American Heart Association 2020 Scientific Sessions. The study was published simultaneously in Circulation.
HARP Results
The aim of the international Women’s Heart Attack Research Program (HARP) study was to enroll women presenting with a diagnosis of MI but no evidence of stenoses 50% or greater on coronary angiography. In all, 301 women at 16 sites were enrolled and 170 were diagnosed with MINOCA during coronary angiography, prompting additional multivessel investigation with OCT followed by CMR within 1 week of the acute presentation.
I think it is very helpful for patients to know what’s wrong with them. Harmony Reynolds
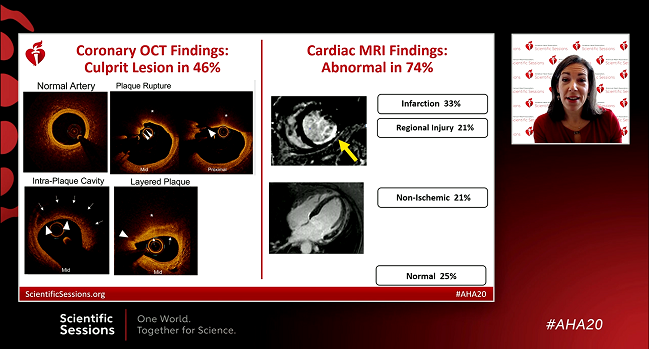
A definite or possible culprit lesion was identified on OCT in 67 of the 145 women (46.2%) who had OCT results of sufficient image quality. Findings included plaque rupture (6%), thrombus without rupture (3%), intraplaque cavity (21%), layered plaque (13%), intimal bump/spasm (2%), and spontaneous coronary artery dissection (1%).
Of the 116 women who also underwent CMR, 86 (74.1%) had abnormal results and 62 (53.4%) had abnormalities pointing to ischemia (infarction or myocardial edema in a coronary territory). A nonischemic pattern was seen in 20.7%, suggesting myocarditis, takotsubo syndrome, or nonischemic cardiomyopathy.
Ultimately, when OCT and CMR results were combined, a plausible cause of MINOCA was identified in a full 84.5% of women; the cause was determined to be ischemic in origin in two-thirds of cases and nonischemic in 21%.
Following her presentation, Reynolds stressed that she didn’t want to underplay the significance of the CMR findings, even if the study’s principal aim had been to identify a cause for ischemic disease. “One in five had a nonischemic, alternate diagnosis and everyone loves to hear that they don't need the whole complement of secondary prevention medications, so that's really important.”
As Reynolds and colleagues note in their paper, only a small percentage of women with MINOCA in HARP had OCT signs of coronary spasm and only one patient was found to have coronary dissection. Of note, however, OCT culprit lesions were less commonly found in women with normal coronary angiograms, and culprit lesions were no more likely to be found in the most-occluded segments. “This is consistent with our previous finding that culprit lesions in women with MINOCA were not usually located at the worst narrowing in that vessel, and suggests that targeting of OCT to specific vessels based on angiographic features may not be useful,” they write. “Clinicians should not dismiss patients with smaller increases in troponin, who are as likely as those with larger increases to have an OCT-defined culprit lesion.”
Asked during the session about the potential utility of IVUS and CT angiography, Reynolds agreed that both may play a role. IVUS, she said, is a decent option at centers without access to OCT, although it’s not yet known how the two intravascular modalities compare in the setting of MINOCA. Cardiac CT can be helpful when angiograms come back normal and there is no option for intravascular imaging, particularly if the patient is reluctant to take a statin.
Caveats and Future Plans
Martha Gulati, MD (University of Arizona, Phoenix), discussant for the HARP results, stressed the strides made in recent years in recognizing this phenomenon, which disproportionately affects women.
“In the past there was no term for this. ‘Normal coronary arteries’ was what people were told and without any obstruction they left with no diagnosis, often told this was a false-positive, and they obviously did not receive any treatment. Now MINOCA is better defined, but as you already saw, MINOCA is not all the same. Technology and imaging can help us understand the pathophysiology, as the HARP investigators demonstrated.”
Finally we can say that this is not just crazy women. Roxana Mehran
Gulati offered a number of caveats, including the fact that the HARP cohort included few STEMI patients, “and we know there is MINOCA in there”; fewer than two-thirds of the cohort had OCT of all three vessels, so the possibility exists that some diagnoses were missed; there was no control group of non-MINOCA patients to see if similar abnormalities could be seen in “normal” arteries; and—“for once”— the cohort didn’t include men, making it impossible to determine if there are any sex-based differences.
Alice K. Jacobs, MD (Boston Medical Center, MA), who moderated a morning press conference, also zeroed in on sex-based differences, asking Reynolds why MINOCA is more frequently diagnosed in women.
Reynolds, in response, called it a “fascinating question,” yet to be answered. “I suspect it has something to do with the balance of blood clotting, with thrombosis and thrombolysis and also perhaps the tendency to spasm [in women versus men], but it’s definitely a very interesting question.”
Commenting on the study for TCTMD, Tom J. Ford, MBChB (Central Coast Local Health District/Gosford Hospital, New South Wales, Australia), praised the study for its strengths—the expertise of the investigators, its prospective, multicenter design, and the fact that it recruited patients prior to angiography. Its chief limitation, he noted, is its observational nature, so it can’t answer the question of whether improved diagnostics lead to changes in care that ultimately improve outcomes.
“I think the message is, if you have ischemic-type chest pain and the troponin has a rise and fall, then the patient has had a myocardial infarction,” he said. “So if we take a step back from all the bells and whistles, the fancy coronary investigations and CMR, at the grass roots level, some of these patients may be falsely reassured in emergency [departments] or by physicians who say look, it's a small troponin rise, it's probably not of any clinical significance, but that patient would potentially need an explanation and also may benefit from treatment. But that would be something we should evaluate in larger studies.”
Reynolds agreed, noting to TCTMD that the CorMicA trial—led by Ford—"focused on the related problem of stable ischemia with nonobstructive coronary arteries, [and] found that quality of life improved in patients given a specific diagnosis and treated for that diagnosis.” HARP, she continued, “was not designed to look at outcomes. I hope these results will set the stage for clinical trials in MINOCA to support stronger recommendations about diagnostic testing, and about medications [and their effect] on outcomes in the future.”
Guidelines and Practice
The 2020 European Society of Cardiology guidelines for non-ST elevation acute coronary syndromes recommend CMR in “all MINOCA patients without an obvious underlying cause,” a class IB recommendation, the authors note. CMR is also recommended in a 2019 AHA scientific statement on the diagnosis and management of MINOCA as well as a 2016 European position paper. All three documents, however, give no formal recommendations on the use of OCT other than to say that intravascular imaging “may be useful” or “valuable” if plaque disruption, plaque erosion, coronary dissection or thrombosis are suspected.
HARP makes the point that OCT insights are likely additive and complementary in this setting. “The finding that 40% of women with normal CMR had an OCT culprit lesion illustrates the potential for OCT findings to change management of MINOCA patients. However, clinical trials are needed to investigate the effects of specific therapies on outcomes.”
Gulati, after the main-event presentation, noted that several guideline documents tend to characterize OCT as an alternative to CMR. “I do think that this needs to be updated,” she said. “This stepwise approach is really important for coming up with the entirety of the reasons” for a MINOCA diagnosis.
Ford pointed out that there are very few ongoing randomized controlled trials of MINOCA patients listed on ClinicalTrials.gov and none—that he was aware of—that are looking at diagnostic strategies as a means to improve outcomes. Without those, he said, it’s unlikely OCT would move up in the guidelines given how confined it is to specialized centers. In some cases, he said, the more-detailed abnormalities picked up on OCT can actually be glimpsed as irregularities or anomalies on coronary angiography. “So in those kinds of patients, there might not be too much additional gain for doing an OCT if you've got an irregularity. You're probably not going to stent it if it's not obstructive.” But it does signal a need for preventive medications.
Demonstrating an effect on hard outcomes would have its challenges, he added, “but I think randomized controlled trials in this population would be helpful to identify the effect on patient understanding of illness, even if we weren't looking at hard outcomes.”
Shelley Wood was the Editor-in-Chief of TCTMD and the Editorial Director at the Cardiovascular Research Foundation (CRF) from October 2015…
Read Full BioSources
Reynolds HR. Coronary optical coherence tomography and cardiac magnetic resonance imaging to determine underlying causes of MINOCA in women. Circulation. 2020;Epub ahead of print.
Disclosures
- Reynolds reports nonfinancial support from Abbott Vascular and Siemens related to the submitted work and non-financial support from BioTelemetry, outside the submitted work.
- Gulati, Jacobs, and Ford report no relevant disclosures.


Comments