ORBITA-2: Angina Phenotype Strongly Predicts PCI Response
A few simple questions that gauge whether symptoms are—or aren’t—typical could provide valuable insights to drive care.
PARIS, France—Stable CAD patients who have angina with typical features are more likely than those who do not to achieve symptom relief from PCI, according to an analysis of data from the ORBITA-2 randomized trial.
The main ORBITA-2 results, published last year in the New England Journal of Medicine, showed that patients randomized to PCI were three times more likely to be free from angina than those assigned to placebo. Still, 60% continued to have symptoms 12 weeks after ischemia had been resolved by PCI.
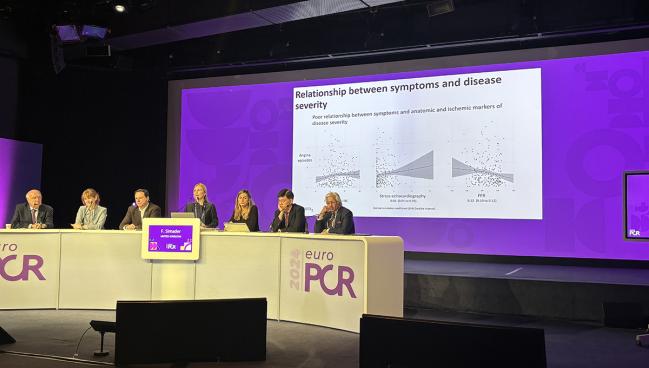
Florentina A. Simader, MD (Imperial College London, England), who presented the new findings here at EuroPCR 2024, said the goal of the current analysis was to ask why.
“While the primary manuscript showed us the overall effect of PCI in all randomized patients,” Simader noted, “perhaps the more important clinical question is: which patients stand to gain the most from PCI and for whom will the effect be less impressive?”
To characterize symptoms, the researchers turned to a decades-old tool: the Rose Angina Questionnaire, developed in 1962. “Rose angina was considered present if patients experienced chest pain during physical activity causing them to slow down or come to a complete stop, with the pain subsiding within 10 minutes,” she explained. “These criteria closely align with more modern guidelines for typical angina,” which the analysis also assessed.
The findings were simultaneously published in the Journal of the American College of Cardiology.
Which patients stand to gain the most from PCI and for whom will the effect be less impressive? Florentina A. Simader
ORBITA-2 gathered information on symptoms directly from patients, on a daily basis, through a smartphone app. Before randomization, the median number of angina episodes was 0.8 per day and the median angina symptom score (calculated to capture angina frequency, use of antianginal drugs, and relevant clinical events) was 4.
“Surprisingly, there was little relationship between symptoms and all markers of disease severity,” including quantitative coronary angiography, stress echocardiography, and fractional flow reserve, Simader reported.
Of the 301 patients randomized in the trial, 267 (89%) had data available from the Rose Angina Questionnaire, with 171 (64%) of those meeting the criteria for Rose angina. With PCI, patients who had this phenotype were more apt to have reductions in angina symptom score (OR 1.9; 95% Credibility Interval [CrI] 1.6-2.0) and in the number of angina episodes (OR 2.1; 95% CrI 1.8-2.4) than those who did not have Rose angina.
Additionally, the patients with Rose angina saw a greater benefit with PCI versus placebo.
ORBITA-2: Impact of PCI vs Placebo
|
|
OR |
95% CrI |
|
Angina Symptom Score Rose Angina Non-Rose Angina |
2.3 1.2 |
2.0-2.7 1.1-1.4 |
|
Number of Angina Episodes Rose Angina Non-Rose Angina |
2.6 1.3 |
2.1-3.2 1.0-1.6 |
“This effect,” said Simader, “was seen immediately postprocedure and sustained throughout 12-month follow-up.”
Two-thirds of the patients with data from the Rose Angina Questionnaire met contemporary guideline-based criteria for typical angina. With PCI, these patients were more likely than those with nontypical angina to reach a better angina symptom score and have fewer angina episodes. And as seen in those with Rose angina, the advantage of PCI over placebo was larger with typical versus atypical angina.
Specific types of angina symptoms also appeared to matter. For instance, heavy pain was a stronger predictor than shortness of breath or shooting pain of whether patients would have symptom improvement with PCI.
“For clinical practice, our results mean that more symptoms do not necessarily indicate worse disease, but the likelihood of symptom improvement with PCI can be assessed at the beginning of the clinical course by acquiring a good history—and the more typical the angina, the greater the expected relief with PCI,” Simader concluded.
Angina is not a trivial matter. It’s disruptive and affects the psychology as well as the physical wellness of our patients. Samir Alam
Samir Alam, MD (American University of Beirut, Lebanon), the presentation’s discussant, praised the ORBITA-2 investigators for their focus on symptoms.
“Yes, I think the case is closed: PCI does ameliorate ischemia and improve symptoms. It improves quality of life. Angina is not a trivial matter. It’s disruptive and affects the psychology as well as the physical wellness of our patients,” he said.
Alam pointed out that the fact that 60% of patients had ongoing symptoms despite PCI is especially counterintuitive given that 80% had single-vessel ischemia to begin with. He questioned what role microvascular dysfunction might have played, though he acknowledged ORBITA-2 did not directly address that.
“Obviously, we know that microvascular disease can coexist with epicardial disease, and it might have contributed to the symptoms of some of our patients. However, this effect would have likely evened out between the groups on the basis of randomization, so we can’t really say,” Simader replied. Another unknown is the distribution of high-risk plaques, and their relevance, since not all participants had CT scans in ORBITA-2.
Lessons for Practice
Rasha K. Al-Lamee, MBBS, PhD (Imperial College London), senior author of the current analysis as well as principal investigator for the ORBITA-2 trial, noted that while the Rose Angina Questionnaire has been around for a long time, it’s mainly as a research tool. “In a way, what I think we’ve done is adapt some of the questions in the Rose into our clinical practice,” so clinicians may not be aware of how those questions came about, she told TCTMD. But “there is a relationship between the Rose and actually what we speak about in terms of typical angina based on the guidelines.”
When applying the lessons from their study in practice, “you would want to incorporate the location of the pain, whether it comes on with exertion, and whether it goes away with rest. Those three key features seem to be the features that encompass typical angina and probably are those features that predict improvement from PCI, she advised.
Also speaking with TCTMD, Simader said that whether angina is described by the term Rose or typical is less relevant than what it means for symptom relief. Both are the kind of “angina that we’re looking for and the pain that will actually improve with PCI, whereas with those atypical presentations, I think the problem is it may not be cardiac at all.”
Clinicians, she continued, “often interpret things through the lens of a stenosis,” meaning that if a patient has known obstructive disease, that’s assumed to be the cause of the symptoms when in fact there might be something else responsible.
In these cases, Simader and Al-Lamee agreed, it’s worth looking for other things causing the pain.
There’s a commonly held belief that women, as well as diabetic patients, tend to have more atypical presentations. So then, there’s the question of whether the relationship between PCI and angina type is consistent irrespective of these factors. The ORBITA-2 investigators did not uncover any higher prevalence of atypical angina in women versus men, or in those with versus without diabetes. However, “it may be underpowered to look at that difference,” Al-Lamee said.
“Fundamentally,” she added, “it’s the typicality of angina that seems to drive the symptom relief with PCI. And so perhaps if cohorts of patients have more atypical symptoms—for whatever reason that might be—they still probably don’t benefit as much from PCI as those with the very typical symptoms that we’ve talked about.”
ORBITA-STAR, another trial by the same research team presented this week at EuroPCR and published in JACC, also points to the key role of symptom assessment in decision-making for stable CAD, Al-Lamee noted.
Christina Lalani, MD, and Robert W. Yeh, MD (both from Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA), in an editorial that accompanies the two papers, note that the large number of patients who did not derive angina relief from PCI in ORBITA-2 “could be viewed as yet another challenge to the therapeutic efficacy of PCI, joining prior studies that have led some to believe that revascularization in stable angina represents low-value care.
“However, careful synthesis of the evidence points to an alternative conclusion: our inability to consistently address angina with revascularization represents a limitation not in our therapeutic capabilities, but rather our diagnostic acumen,” they write. “We have no tests that reliably identify the connection (or lack thereof) between a patient’s symptoms and coronary anatomy.”
The ORBITA-2 data thus address a crucial need, the editorialists say.
“Against a background of rapidly changing technology, an important solution may be found simply in taking more careful histories from our patients,” they write. “Looking forward, as we innovate in our therapies for the treatment of angina, it is critical that we concurrently strive toward building evidence-based strategies to identify the link between a given patient’s symptoms and their observable disease. In doing so, we will create the best opportunity to offer personalized and targeted care for the diverse patient population presenting with chest pain.”
Caitlin E. Cox is Executive Editor of TCTMD and Associate Director, Editorial Content at the Cardiovascular Research Foundation. She produces the…
Read Full BioSources
Simader FA, Rajkumar CA, Foley MJ, et al. Symptoms predict efficacy of percutaneous revascularization in patients with stable ischemic heart disease. J Am Coll Cardiol. 2024;Epub ahead of print.
Lalani C, Yeh RW. Residual chest pain after PCI – a failure in diagnosis rather than treatment. J Am Coll Cardiol. 2024;Epub ahead of print.
Disclosures
- Simader reports sponsorship from Servier Pharmaceuticals.
- Al-Lamee reports serving on the advisory boards of Janssen Pharmaceuticals, Abbott, and Philips, and receiving speaker’s honoraria from Abbott, Philips, Medtronic, Servier, Omniprex, Menarini.
- Lalani reports no relevant conflicts of interest.
- Yeh is a consultant for and has investigator-initiated research grants from Abbott Vascular, Boston Scientific and Medtronic, and is a consultant for CathWorks, Elixir Medical, Shockwave, and Zoll.




Comments