PCI With Intravascular Imaging or Functional Testing Bests Angiography Alone
(UPDATED) The benefit was seen in ACS and non-ACS patients, lending more support for adjunctive tests to guide PCI.

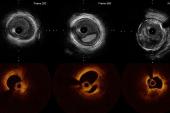
The meta-analysis, which included 32 randomized, controlled trials with more than 22,600 patients, showed that functionally guided PCI with primarily fractional flow reserve (FFR) or instantaneous wave-free ratio (iFR), as well as intravascular imaging using IVUS or optical coherence tomography (OCT), outperformed angiography-guided PCI alone for reducing MACE over follow-up ranging from 6 months to 5 years.
Currently, functional testing with FFR or iFR is a class 1 recommendation to help guide decisions around PCI, while use of IVUS is a class 2a recommendation to help reduce the risk of ischemic events in left main CAD or complex coronary lesions, with optical coherence tomography (OCT) considered a reasonable alternative to IVUS.
Lead investigator Toshiki Kuno, MD, PhD (Montefiore Medical Center/Albert Einstein College of Medicine, New York, NY), believes that based on all the evidence to date, intravascular imaging could have a more prominent role in the American College of Cardiology/American Heart Association/Society for Cardiovascular and Angiographic Interventions (ACC/AHA/SCAI) revascularization guidelines.
“IVUS should be a class 1 recommendation,” Kuno told TCTMD.
The study also helps shed some light on how intravascular imaging, employed to optimize the placement of the stent, stacks up against functional testing used to determine the physiologic significance of a coronary stenosis. In the large randomized trial, FLAVOUR, functional imaging with FFR was noninferior to intravascular imaging with IVUS when it came to the primary endpoint of death, MI, or revascularization at 24 months.
“There are very few studies comparing intravascular vascular imaging-guided PCI versus functional guided PCI,” said Kuno, noting that IVUS in FLAVOUR was used like FFR in that operators deferred PCI based on mean lumen area. “Given only a few studies available, indirect comparisons using a network meta-analysis may be useful but the limitation would be combining studies of IVUS for [stent] optimization and [PCI] deferral,” he said. While this analysis didn’t show any significant difference in terms of the primary endpoint in a head-to-head comparison, ranking the outcomes tended to favor intravascular imaging.
Benefit Also Seen in ACS
The use of intravascular imaging remains infrequent in the US compared with Japan, said Kuno. Estimates suggest that only 15% of PCIs in the United States are performed with adjunctive intravascular imaging whereas, in Japan, that number is closer to 90% and has been part of standard practice since 2010. Earlier this year, the ACC Interventional Council stated that use of intracoronary imaging should now be routinely used by operators.
“The US is delayed by more than a decade compared to Japanese practice,” said Kuno. “Of course, there are a lot of reasons for the delay, but the main point seems to be that operators may not like to use it.” In addition to physician preference, hospital culture, lack of training, and costs are also significant factors limiting widespread use.
The current meta-analysis, which was published in the Journal of the American College of Cardiology, sought to address how invasive functional test and intravascular imaging compared against angiography alone, and included such trials as FAME, ULTIMATE, ILUMIEN III, FLOWER-MI, TARGET-FFR, FLAVOUR, RENOVATE-COMPLEX-PCI, and ILUMIEN IV, among others. The definition of MACE varied, but typically included mortality (either all-cause or cardiovascular), MI, and need for target lesion or vessel revascularization.
In the pooled dataset, intravascular imaging-guided PCI was associated with a significant 28% lower risk of MACE compared with angiography alone. It was also associated with a 44% lower risk of cardiovascular mortality, a 19% lower risk of MI, a 52% lower risk of stent thrombosis, and a 25% lower risk of target lesion revascularization when compared with angiography alone. Alternatively, functionally guided PCI was associated with a 19% lower risk of MACE and a 22% lower risk of MI compared with angiography alone, with no effects observed on cardiovascular mortality, stent thrombosis, or target lesion revascularization.
Comparing intravascular imaging with functionally guided PCI, Kuno and colleagues saw no significant differences in any endpoints. Although there were few trials comparing intravascular to functional imaging—the lone randomized trial being FLAVOUR—researchers ranked the three strategies and found that IVUS/OCT came out on top for decreasing the risk of MACE, cardiovascular death, stent thrombosis, and target lesion revascularization.
That does not mean that IVUS- or OCT-guided PCI will be beneficial in every case, Kuno said. “Evidence for IVUS is coming from [studies] of more complex or diffuse lesions, long stents, or bifurcations,” which is a subset of patients where angiography alone is really challenging, he added. “I'm not sure we can say that we should use IVUS for all PCI lesions—it might not be necessary for simple lesions. This is a meta-analysis so some of baseline patient characteristics are quite different, especially in the intravascular imaging guided PCI group.”
Of the 32 randomized trials, 19 were studies of patients with ACS, and the results in this population were similar to the overall findings. Sripal Bangalore, MD (NYU Langone Health, New York, NY), the study’s senior author, said that the reason they performed this analysis is that there were trials, such as the FLOWER-MI trial in STEMI patients and FUTURE, which included a mix of ACS and non-ACS patients, that didn’t show any advantage with functional testing. The hypothesis for why those trials were negative was that plaque burden and morphology may be more important in the ACS setting than functional significance.
“We showed that in both ACS and non-ACS setting, imaging-guided PCI was the best strategy,” he told TCTMD in email.
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Kuno T, Kiyohara Y, Maehara A, et al. Comparison of intravascular imaging, functional, or angiographically guided coronary intervention. J Am Coll Cardiol. 2023;Epub ahead of print.
Disclosures
- Kuno reports no conflicts of interest.
- Bangalore is an advisory board member for Abbott Vascular, Biotronik, Amgen, Pfizer, and Reata.




Comments