Percutaneous Edge-to-Edge Repair for Tricuspid Regurgitation: Some Successes, Some Caveats
The largest series to date of patients treated with MitraClip in the tricuspid position appears in a special journal issue focused on valve interventions.
Transcatheter edge-to-edge repair of tricuspid regurgitation appears to reduce mortality and heart failure hospitalizations in patients at high surgical risk, according to the largest series to look at procedural and clinical outcomes in this very sick patient group.
The paper is one of a series of publications focused on percutaneous interventions for tricuspid regurgitation (TR) appearing today in a special issue of JACC: Cardiovascular Interventions.
Percutaneous edge-to-edge leaflet coaptation was originally developed for mitral regurgitation (MR) but has more recently been offered to severely ill patients at prohibitive surgical risk. Other transcatheter approaches—including coaptation, annuloplasty, and caval devices, as well as full percutaneous replacement valves—are a hot area of investigation. But as Christian Besler, MD (University Hospital, Leipzig, Germany), and colleagues write, the now considerable experience with the MitraClip device (Abbott)for MR has made it the most commonly used approach in the tricuspid position.
Besler et al’s series includes 117 patients with severe symptomatic TR treated with a MitraClip at one of two centers in Germany. Seventy-four of the patients also had severe mitral regurgitation and underwent MitraClip repair of the mitral valve during the same procedure.
In the tricuspid position, 185 clips were deployed at the anteroseptal commissures and 34 clips at the posteroseptal commissures. Procedural success, defined as a reduction in TR grade of 1 or more within 30 days, was achieved in 81% of patients, with median TR effective regurgitant orifice area reduced from 0.5 cm2 to 0.2 cm2. Over a median follow-up of 184 days, 21 patients were readmitted for heart failure and 24 patients died. Of note, procedural success was an independent predictor of time free from death and failure (HR 0.20; 95% CI 0.08-0.48).
“Even though it’s early days and it's off-label use, MitraClip seems to work,” said Philipp Lurz, MD, PhD (University Hospital, Leipzig), who is a joint senior author along with Jörg Hausleiter, MD (Klinikum der Universität München, Munich, Germany). “Clip implantation in the tricuspid position is feasible and effective in reducing TR in a high number of patients,” he told TCTMD. “This is an important finding.”
The paper by Besler, Lurz, and colleagues also offers new insights into morphologic predictors of MitraClip success for TR. In multivariate models, the only echocardiographic features that predicted procedure success were a smaller tricuspid valve coaptation gap—7.2 mm appeared to be the cutoff—and presence of a central/anteroseptal TR jet. Patients with gaps less than 7.2 mm with a main TR jet that was central/anteroseptal had a combined success rate of 92%. By comparison, patients with gaps larger than 7.2 mm, in whom the main TR jet as noncentral/nonanteroseptal, had a success rate of zero.
“Jet orientation matters,” Lurz said. “When the main TR jet is located centrally or between the anterior and septal leaflet, that's a good thing, because clip position between the anterior and septal leaflet was something which is technically feasible and it works quite well, whereas clip placement between posterior and anterior is technically more difficult and also it seems that it is less effective in reducing the annular dimensions and pulling everything together.”
According to Lurz, this is the first time, in a reasonably sized cohort, that investigators have been able to provide clues as to what morphological conditions might help predict which patients with TR will benefit from a MitraClip. More than that, he said, “this is the first time that there is some [strong] evidence pointing towards a clinical benefit of treating TR alone. Successful TR treatment was associated with better survival than unsuccessful, and this is important because there is always the question of whether TR is just a bystander—a sign of more severe disease—or whether it's an [independent] contributor to adverse outcomes.
TR a Culprit in Unsuccessful MR Repair?
In a separate paper also published in the same issue of JACC: Cardiovascular Interventions, Besler and Lurz, the first and senior author, respectively, looked at patients with both MR and TR who underwent isolated MitraClip implantation in the mitral position as compared to edge-to-edge repair in both the mitral and tricuspid valves. While the numbers were small (34 versus 27, respectively) the authors show that while the reduction in MR was similar in both groups, heart failure hospitalizations were significantly reduced among patients who had both forms of regurgitation as compared with patients who only underwent mitral edge-to-edge repair.
“This can shed some light on the difficult story of concomitant mitral and tricuspid regurgitation,” Lurz told TCTMD. “Cardiac output only improves when you treat both valves, which might explain the worse outcomes in patients with both tricuspid and mitral regurgitation, and points us in a direction where one could imagine that, in the future, it might make sense to treat both valves.”
Enthusiasm for TR Progress
Both of the Besler et al papers were greeted with enthusiasm by accompanying editorials. Florian Deuschl, MD, and Ulrich Schäfer, MD (University Hospital Hamburg-Eppendorf, Germany), in response to the larger TR series, write: “Besler et al elegantly prove not only feasibility of an edge-to edge repair in TR patients, they also show the direct benefit of procedural success on outcome and provide the first evidence regarding predictors for favorable outcome of interventional TR treatment. A procedural success of 81% is remarkable when considering the challenges of tricuspid valve imaging and the fact that the device used is not specifically designed for tricuspid valve intervention.”
In an editorial accompanying the second paper, comparing the isolated mitral edge-to-edge repair with combined repair, Hausleiter along with Daniel Braun, MD (Klinikum der Universität München, Germany), who is also a co-author on the first paper, conclude that the data “provide an important basis for further randomized trials following approval of edge-to-edge repair systems for severe TR.”
The best combination of approaches as well optimal timing of procedures will depend on the future availability of the range of devices currently under study, they add.
In a state-of-the-art paper, published online today in the Journal of the American College of Cardiology, Lluis Asmarats, MD (Quebec Heart & Lung Institute, Laval University, Quebec City, Canada), colleagues observe that the off-label use of the MitraClip has become “the first-choice approach for high-risk patients with functional TR, likely because of wide availability and operator familiarity. More than 650 procedures have already been performed worldwide, and patients receiving this therapy represent > 50% of patients included in the first international registry assessing different available transcatheter TR devices.”
But a much wider range of percutaneous repair and replacement devices are at different stages of development they note.
“Although the field is still in its infancy, multiple studies have already shown the feasibility and safety of different transcatheter TV therapies,” Asmarats et al write. “The recent first-in-human cases of orthotopic transcatheter tricuspid valve repair, with no or minimal residual TR in most cases, represent a landmark step forward in the transcatheter treatment of TR. Steady device innovation and iteration together with increased experience are anticipated to improve procedural and clinical outcomes in the coming years.”
TR affects an estimated 1.5 million people in the United States alone, with a yearly incidence of 200,000 patients, the review points out. That number soars to more than 300,000 in Europe, say Asmarats and colleagues, adding that TR is “most often functional”—a late marker for end-stage chronic heart failure.
Next Steps
Samir Kapadia, MD (Cleveland Clinic, OH), one of the associate editors for JACC: Cardiovascular Interventions, spoke with TCTMD about the papers published in the special issue this week, which he said was an effort to capture the excitement felt by investigators in the fast-moving field of tricuspid valve innovation. A key hurdle, said Kapadia, is that all of the devices currently being pioneered in this space are being tested in patients with extremely advanced disease.
“This is the main challenge. When you are doing something innovative and new, you want patients who are symptomatic,” but not so sick that they can’t withstand the procedures, he said. As new devices move from first-in-human and compassionate-use series to clinical trials, Kapadia said he would like to see studies enrolling patients with tricuspid regurgitation much earlier.
“There are a lot of patients who could be helped by this—isolated TR is not an uncommon problem,” he pointed out. “But what state we are intervening in these patients is a real challenge. . . and whether patients, doctors, and regulatory bodies will be willing to do these procedures in relatively ‘well’ patients is the big question. Because that’s where we have to go in order to see some success. The first step is to establish the safety of the devices in very sick patients, but there the efficacy is very hard to judge. So we need to judge the safety of the device first, then take the device to a less advanced disease population and try to test it for efficacy. That would be one of the approaches, but it’s easier said than done.”
Both Kapadia and Lurz, speaking with TCTMD, also added a note of caution to operators considering offering MitraClip to patients with isolated tricuspid regurgitation. Both stressed that the current iteration of the device was designed for different anatomy and requires much more careful navigation and positioning, as well as a detailed understanding of what Lurz termed “the very crowded subvalvular apparatus.”
Kapadia agreed, calling TR edge-to-edge repair both a “challenge” and “an opportunity.”
“There are enough differences between the mitral and tricuspid valves that make the tricuspid a real learning curve,” he said. “It is not a given that if you are very good with the MitraClip that you have learned enough—you need to learn a bit further.”
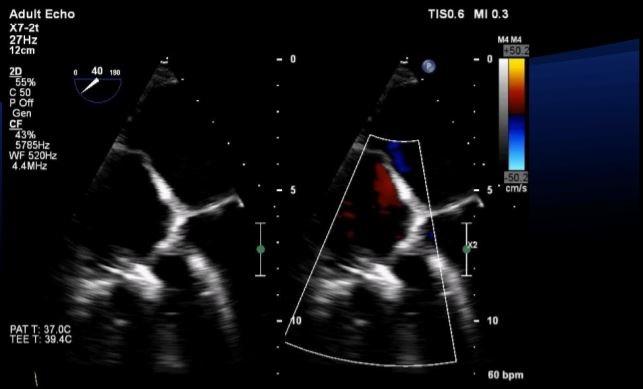
Photo Credit: Rebecca Hahn. Intraprocedural Imaging For Tricuspid Valve Interventions. Presented at: ECHO 2018. April 20, 2018. New York, NY.
Shelley Wood was the Editor-in-Chief of TCTMD and the Editorial Director at the Cardiovascular Research Foundation (CRF) from October 2015…
Read Full BioSources
Besler C, Orban M, Rommel K-P, et al. Predictors of procedural and clinical outcomes in patients with symptomatic tricuspid regurgitation undergoing transcatheter edge-to-edge repair. J Am Coll Cardiol Intrv. 2018;11:1119-1128.
Besler C, Blazek S, Rommel K-P, et al. Combined mitral and tricuspid versus isolated mitral valve transcatheter edge-to-edge repair in patients with symptomatic valve regurgitation at high surgical risk. J Am Coll Cardiol Intrv. 2018;11:1142-1151.
Deuschl F, Schäfer U. Tricuspid valve regurgitation: a challenge for interventional treatment. J Am Coll Cardiol Intrv. 2018;11:1129-1130.
Hausleiter J, Braun D. Mitral meets tricuspid: is severe tricuspid regurgitation a bystander or is there a need for combined percutaneous mitral and tricuspid valve repair? J Am Coll Cardiol Interv. 2018;Epub ahead of print.
Asmarats L, Puri R, Latib A, et al. Transcatheter tricuspid valve interventions: landscape, challenges, and future directions. J Am Coll Cardiol. 2018;71:2935-2956.
Disclosures
- Braun reports receiving speaker honoraria and travel support from Abbott.
- Deuschl reports receiving speaker honoraria from Abbott.
- Hausleiter reports receiving speaker honoraria and travel support from Abbott Vascular and Edwards Lifesciences.
- Kapadia reports serving on the advisory board of NaviGate and having stock options in NaviGate Cardiac Structures.
- Lurz reports serving as a consultant to and receiving speakers’ honoraria from Abbott Vascular.
- Schäfer reports serving as a proctor and consultant to Abbott Vascular and has also received speaker honoraria, travel support, and study grants from Abbott Vascular.


Comments