RAPCO: Radial Artery Beats Both RITA and Vein Grafting at 15 Years
The findings might not be generalizable given a high exclusion rate, variations in practice, and statistical issues, experts say.
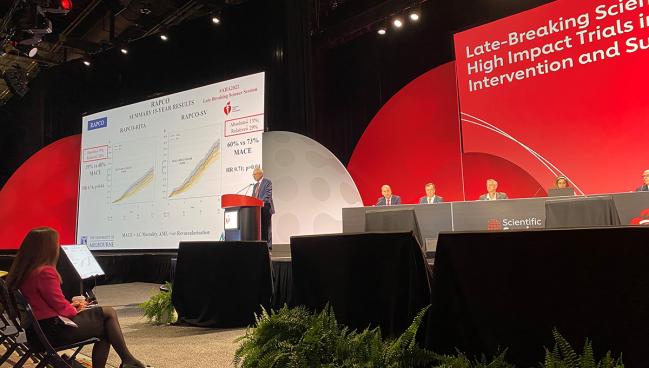
CHICAGO, IL—For patients undergoing coronary artery bypass grafting, use of radial arteries leads to less MACE over 15 years compared with using either right internal thoracic artery (RITA) or saphenous vein grafts, according to randomized data from RAPCO.
Several observational trials and meta-analyses have demonstrated a benefit of radial artery grafts in CABG, but the data from RAPCO are the first to come from a single trial and represent some of the longest follow-up yet to inform practice, with some patients having been randomized nearly 25 years ago. These latest findings from RAPCO show 9% and 13% absolute risk reductions for MACE with radial artery over RITA and saphenous vein grafting, respectively.
“We now have single trial data, which is very important in terms of outcomes,” said David Hare, MD (University of Melbourne, Australia), who presented the findings here today in a late-breaking clinical trial session at the American Heart Association (AHA) 2022 Scientific Sessions. “For me, that suggests that all isolated CABG operations should consider using a radial graft if it's actually suitable unless there are specific contraindications.”
One big caveat is that the original trial was designed with the primary endpoint of graft patency, with a nonpowered co-primary endpoint of overall survival. Making that point to TCTMD, Faisal Bakaeen, MD (Cleveland Clinic Foundation, OH), noted that the current analysis included all-cause mortality in the study’s definition of MACE.
But with all-cause mortality on its own: “This primary endpoint remains negative at 15 years,” Bakaeen said in an email.
Discussing the findings following the presentation, Marc Ruel, MD (University of Ottawa Heart Institute, Canada), called the long-term follow up of RAPCO patients “quite impressive.” However, he noted the relatively high and “humbling” rate of MACE in all groups, which was likely reflective of the older age of patients as well as the inclusion of all-cause compared with cardiovascular death in the trial’s definition of MACE.
RAPCO-RITA and RAPCO-SV
For the study, Hare and colleagues conducted a two-part analysis comparing radial artery grafting to using the free RITA in patients younger than 70 (or younger than 60 with diabetes) or saphenous vein grafting in patients 70 or older (or 60 or older with diabetes). MACE was defined as all-cause mortality, acute MI, or repeat revascularization.
In the RAPCO-RITA analysis, 394 patients (mean age 59 years; 11% diabetes) were randomized to receive radial artery (n = 198) or free RITA grafting (n = 196), with 15-year clinical follow-up data available in all but one patient in the radial artery group. The MACE rate was significantly lower over 15 years in those who received radial artery grafting (39.4% vs 48.5%; HR 0.74; 95% CI 0.55-0.97), driven by a trend in lower all-cause mortality (22.2% vs 30.1%; HR 0.69; 95% CI 0.47-1.02).
For the RAPCO-SV side of the trial, 225 patients (mean age 73 years; 45% diabetes) were randomized to receive radial artery (n = 113) or saphenous vein grafting (n = 225), with 15-year clinical data available in all but one patient in the saphenous vein graft group. Again, the MACE rate was significantly lower for radial artery grafting over 15 years (60.2% vs 73.2%; HR 0.71; 95% CI 0.52-0.98), and this was also driven by lower rates of mortality (52.2% vs 63.4%; HR 0.74; 95% CI 0.52-1.04).
There were no differences observed in the individual secondary endpoints of MI or repeat coronary revascularization for both analyses. Additionally, prespecified subgroup analyses looking at age, sex, and diabetes status were all consistent with the main findings, although there was a trend toward benefit with radial artery grafting for females in the RAPCO-SV results.
Generalizability Issues
Bakaeen, to TCTMD, noted that because the trial has “reported multiple previous interim analyses published in various journals over the years [with] no adjustments for multiple testing here . . . the current conclusions are far from definitive” and the statistics presented today “cannot be taken at face value.”
Bakaeen also pointed out several issues with RAPCO’s generalizability. “RAPCO is a small, single-center trial performed by RA-centric surgeons,” he said. “It is not convincing that all RITAs could have reached the intended most important non-LAD target taken as free grafts off the aorta. A composite RITA-LITA is often needed to enhance the reach of RITA, but this was never used in RAPCO. This raises the possibility that RAPCO surgeons may have disadvantaged RITA to make it more like the more familiar RA conduit.”
Because of this, he continued, surgeons may have settled for a “a less important, but more reachable RITA target instead of the prespecified and more important study target,” which would have ultimately disadvantaged RITA against radial artery grafts. The fact that there was a high rate of crossover from the RITA arm is “probably a reflection of relative RITA inexperience,” Bakaeen said.
Additionally, about two-thirds and three-quarters of potential patients in the RAPCO-SVG and RAPCO-RITA analyses, respectively, were excluded from enrollment. “The patients were generally fit with minimal comorbidities compared to typical CABG patients that we see nowadays,” Bakaeen said. This “further weakens the generalizability of this study.”
Ruel, too, pointed out some issues that might have disadvantaged RITA grafts. Because the study was not blinded, he said, “postrandomization care might have differed even at the time of surgery.” Also, “using the free RITA is slightly more difficult than using the saphenous vein or radial artery,” indicating that the results may not have been balanced accordingly, he suggested.
Moreover, Ruel continued, “the radial artery versus RITA results are concerning because biologically the RITA should provide graft durability.”
In fact, Hare, too, said that his initial hypothesis was that the RITA grafts would end up being better than those that were used the radial arteries. “I was surprised,” he said.
Hare explained that they used aorta coronary grafts in order to “standardize the standard operation, which was the LITA to the LAD. So we had to have the RITA reach anywhere in the circumflex or right territory,” he said. “In terms of difference between whether it was going to the circumflex or to the right coronary circulation, [there was] no difference in that.”
Also, Hare noted that all patients regardless of graft type were referred to an “independently run secondary prevention cardiac rehab program which was quite separate to the trial and they all got identical treatment.”
Yael L. Maxwell is Senior Medical Journalist for TCTMD and Section Editor of TCTMD's Fellows Forum. She served as the inaugural…
Read Full BioSources
Hare DL. Radial artery patency and clinical outcomes study – RAPCO: the 15-year RCT clinical outcomes comparing radial artery with right internal thoracic artery or with saphenous vein. Presented at: AHA 2022. November 6, 2022. Chicago, IL.
Disclosures
- RAPCO was funded by the Heart Foundation (Australia).
- Hare reports receiving payment for research projects, consultancies, travel, advisory boards, and/or lecture fees from Abbott, Amgen, AstraZeneca, Bayer, Boehringer-Ingelheim, CSL-Biotherapies, Lundbeck, Menarini, Merck, Pfizer, Regeneron, Sanofi, Servier, and Vifor.
- Bakaeen reports no relevant conflicts of interest.




Comments