Ross Procedure Done Well Holds Up Over Time
A look at nearly 1,500 patients shows that, with experience, the operation can offer “excellent” results, researchers say.

When done well, the Ross procedure can offer young and middle-age adults good survival and steady hemodynamic outcomes over the long term, according to an observational study of nearly 1,500 patients.
“There is no ideal valve substitute for young adults requiring aortic valve replacement,” its authors say. Mechanical valves require permanent anticoagulation, while bioprosthetic valves can result in repeat interventions in these patients, who are likely to live for several decades.
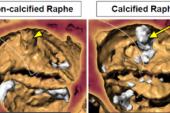
With the Ross procedure, the aortic valve is removed and then replaced with the patient’s own pulmonary valve. The latter is then replaced with a donor valve. The Ross procedure is relatively rare compared with other fixes for aortic valve dysfunction, the investigators note in JAMA Cardiology. They attribute “lagging interest” to the complexity of the initial procedure, which can be overcome by experience, as well as the fear that both the aortic and pulmonary valves might fail in a patient who initially had only had single-valve disease.
There’s also the question of what role the Ross procedure would play if TAVI use were to dip below the current guideline-recommended age cutoff of 65.
It would be good for patients if the Ross procedure got more attention. Mostafa M. Mokhles
Mokhles pointed out that current guidelines don’t reflect the existing literature that supports the Ross procedure. In the United States, for example, the 2020 valvular heart disease guidelines give it a class IIb recommendation (level of evidence B), specifying that the intervention “typically is reserved for younger patients with appropriate anatomy and tissue characteristics in whom anticoagulation is either contraindicated or undesirable, and it is performed only at Comprehensive Valve Centers by surgeons experienced in this procedure.”
“It would be good for patients,” Mokhles suggested, “if the Ross procedure got more attention.”
Gilbert Tang, MD (Mount Sinai Health System, New York, NY), commenting on the results for TCTMD, said one reason the Ross procedure isn’t often discussed in adults is because historically it has mainly been done in pediatric patients.
Regarding the potential for wider adoption, he stressed that “the outcomes of the operation and the durability is highly dependent on the surgeon or the surgical team’s experience, as well as their expertise.” As such, the outcomes seen here might not extend to centers that are not as proficient in the procedure. He also cautioned that patients shouldn’t delay seeking care in the pursuit of obtaining the Ross procedure when other options are more readily available where they live.
Even so, “in expert hands, it’s an excellent operation,” Tang said, one that can restore life expectancy “as if they’d never had this disease. At the same time, it has to be selected carefully and done in the right patients.”
Vast Majority Alive at 15 Years
Led by Jamie L. R. Romeo, MD, PhD (Erasmus Medical Centre, Rotterdam, the Netherlands), the investigators looked at the outcomes of 1,431 patients (74.3% men) who had undergone the Ross procedure at a median age of 48.5 years (range, 18.1 to 65 years). Among the 1,022 with known valve morphology, 76.1% had a bicuspid aortic valve. Patients were treated at one of five experienced centers between 1991 and 2018, with a median follow-up period of 9.2 years; the data set spanned 13,015 patient-years.
Implantation techniques varied. Root inclusion was performed in 24.9%, root replacement in 34.0%, and subcoronary implantation in 41.1%. For nearly all patients (98.6%), right ventricular outflow tract reconstruction was done with homografts, while a minority received bioprostheses.
In-hospital survival was 99.3%. By 10 years, 95.1% of patients had survived. And by 15 years, 88.5% were still alive. For cardiac mortality, freedom from death was 98.6% at 10 years and 96.5% at 15 years. Several characteristics were associated with increased death risk, including older age at operation, female sex, and preoperative peripheral vascular disease, chronic obstructive pulmonary disease, congenital heart disease, and congestive heart failure.
Freedom from autograft reintervention at 15 years was 92.0%. Freedom from homograft reintervention was 97.2% over the same time span. Late events included autograft endocarditis (0.11% per patient-year), homograft endocarditis (0.08% per patient-year), and stroke (0.3% per patient-year).
Echocardiographic measurements were available for 82.8% of patients after their Ross procedures. Approximately 1% were estimated to experience moderate or severe autograft regurgitation by 20 years. The likelihood a patient would develop significant regurgitation did not depend on whether they had moderate or severe aortic valve regurgitation prior to their surgery, nor was it associated with surgical technique.
For the homograft, “the gradient initially increases during the first postoperative decade, after which it slopes down and plateaus during the second postoperative decade,” the researchers note, adding that female sex was linked to a lower gradient but increased odds of significant postprocedural regurgitation. The complication was less common in patients who received a homograft versus bioprosthesis to replace their pulmonary valve and in those whose homografts were from older versus younger donors.
Should There Be a Ross Renaissance?
JAMA Cardiology Editor Robert O. Bonow, MD (Northwestern University, Chicago, IL), and Deputy Editor Patrick T. O’Gara, MD (Brigham and Women’s Hospital, Boston, MA), add their own perspective.
“These results are noteworthy and indicate what can be achieved by excellent surgeons in centers devoted to this procedure in patients who are appropriately selected,” they write in an editor’s note. “However, this experience may not be generalizable beyond this small network of specialized centers, because it is unlikely that these results currently could be replicated more broadly in other academic institutions and community hospitals. These results do call for further randomized clinical trials to determine whether the Ross procedure can achieve its potential benefits in young patients in need of AVR.”
Mokhles agreed that randomized controlled trials comparing Ross to other options are needed before the procedure gains wider acceptance, a sentiment also expressed by Tang.
You have a living autologous valve that is a mirror image of a normal aortic valve in the aortic position, versus having something that is just nonliving. Ismail El-Hamamsy
Ismail El-Hamamsy, MD, PhD (CHU Sainte Justine, Montreal, Canada), a study co-author, said a strength of the Ross procedure is that “you have a living autologous valve that is a mirror image of a normal aortic valve in the aortic position, versus having something that is just nonliving.”
Interest in Ross has already been growing, he observed. “What we’ve seen over the last 10 years or so is accumulating evidence that consistently seems to show that, when it comes to nonelderly adults, the Ross procedure really allows for patients to have optimal long-term outcomes versus prosthetic aortic valve replacement, whether that be with a biological valve or a mechanical valve.”
As TAVI extends to younger, lower-risk patients, might it overlap with the Ross procedure? Maybe one day, said El-Hamamsy, but not yet. “I would say it’s a different population, although there’s a lot of creep in terms of the age range at which TAVRs are being proposed or even performed,” he commented. “There’s still a long ways to go before we can safely say that TAVR is a reasonable option in patients under 60.
“The Ross is really mainly aimed for patients under 60; in other words, patients that have an anticipated life expectancy of 15 years or more definitely stand to benefit from having a Ross versus a prosthetic valve replacement, whether that be open or transcatheter,” he explained.
El-Hamamsy, who’s now based at Mount Sinai Hospital in New York, said that he’s seen a “Ross renaissance” as of late, one that’s brought him to various hospitals across the United States, Europe, Canada, and China to share his knowledge. “In the last 5 years, I’ve been to at least 15 centers,” El-Hamamsy said, adding, “I think lessons have been learned from the initial Ross enthusiasm in the 90s, where every Tom, Dick, and Harry was trying to do Rosses and [hurting] patients, unfortunately. Now we understand that that should be concentrated in certain hands and certain centers.”
What’s required are continued training that results in regional centers of excellence as well as “transparent reporting of outcomes so that patients know where to go or where not to go,” he said.
Caitlin E. Cox is News Editor of TCTMD and Associate Director, Editorial Content at the Cardiovascular Research Foundation. She produces the…
Read Full BioSources
Romeo JLR, Papageorgiou G, da Costa FFD, et al. Long-term clinical and echocardiographic outcomes in young and middle-aged adults undergoing the Ross procedure. JAMA Cardiol. 2021;Epub ahead of print.
Bonow RO, O’Gara PT. Reconsidering the Ross procedure. JAMA Cardiol. 2021;Epub ahead of print.
Disclosures
- Mokhles is funded by an NWO Veni grant from the Netherlands Organisation for Scientific Research.
- Romeo, El-Hamamsy, and Bonow report no relevant conflicts of interest.
- Tang reports being a physician proctor for Medtronic as well as a consultant to Medtronic, Abbott, and Gore.
- O’Gara reports serving on executive committees for the APOLLO Transcatheter Mitral Valve Replacement Trial (Medtronic) and the EARLY TAVR Trial (Edwards Lifesciences) outside the submitted work.




Comments