Stepwise DAPT De-escalation Shows Promise in DCB-Only PCI for ACS
The first trial to test shortened DAPT in coronary DCBs, REC-CAGEFREE II builds upon the evidence available for DES PCI.

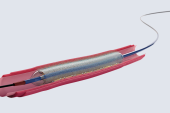
PARIS, France—The first trial to test a plan for de-escalating dual antiplatelet therapy (DAPT) after drug-coated balloon (DCB) angioplasty in ACS patients has shown that, like similar studies with stents, a less-is-more strategy is feasible and safe.
In the randomized REC-CAGEFREE II study of DCBs in ACS, a strategy using aspirin and ticagrelor through 1 month, then ticagrelor alone through 6 months, followed by aspirin alone through 12 months was noninferior to standard 12-month DAPT for a composite endpoint of net adverse clinical events (NACE).
The study showed that “this theory is correct, and the hypothesis has been tested; it’s valid” in patients with STEMI, NSTEMI, or unstable angina, co-author Chao Gao, MD (Xijing Hospital, Xi’an, China), told TCTMD. Could this regimen be applied to all patients eligible for PCI with DCB? “I still don't know the answer because this is a trial from China, it's only an East Asian population, and that's not representative of how it is in the States or in Europe,” he added.
The REC-CAGEFREE II results “provide the first piece of evidence investigating a tailored antiplatelet regimen for patients with DCB,” said Ling Tao, MD, PhD (Xijing Hospital), who presented the findings in a late-breaking clinical trial session today at EuroPCR 2024. “If all clinically relevant ischemic or bleeding events were considered by hierarchical clinical importance, an overall benefit would have been seen with the stepwise DAPT de-escalation compared with the standard 12-month DAPT.”
Discussing the study, Thomas Cuisset, MD, PhD (CHU Timone, Marseille, France), said that on top of the findings seen in a variety of DAPT studies in DES patients, including TWILIGHT and TICO, the results of the current study will encourage him to “use more de-escalation for ACS patients, and I would say regardless of the PCI strategy, whether my patient has been treated with DES or with DCB.”
However, Robert Byrne, MBBCh, PhD (Mater Private Network, Dublin, Ireland), who also served as a discussant during the session, told TCTMD he’s not yet ready to make any changes to his practice. The fact that the study population was dominated by unstable angina patients, at about 60%, rather than more serious ACS patients, raises the question of generalizability, he said. “But [it’s] a step in the right direction because finally it's drug-coated balloon angioplasty patients being randomized to different DAPT durations.”
Ajay Kirtane, MD (NewYork-Presbyterian/Columbia University Irving Medical Center, New York, NY), told TCTMD it seems reasonable that patients treated with DCBs for de novo lesions might benefit from shorter DAPT durations. “If I treated a distal vessel lesion or side branch with bifurcation, I think a month is sufficient,” he said, adding that these patients will be rare in the US according to device indications at the moment.
DAPT De-escalation Noninferior
For the investigator-initiated study, Tao, Gao, and colleagues included 1,948 patients (mean age 59 years; 75% male) with STEMI, NSTEMI, or unstable angina who were considered suitable for PCI with DCB-only treatment and underwent the procedure at 41 institutions in China. Patients were randomized to standard 12-month DAPT with ticagrelor and aspirin (n = 973) or stepwise de-escalation following 1 month of DAPT to ticagrelor only and switching again to aspirin only at 6 months (n = 975).
About one in five patients were considered to be at high bleeding risk, and 30.5% had diabetes. The main reasons for receiving DCB treatment included single-vessel disease (55.9%), bifurcations (45.4%), ISR (18.6%), and diffuse lesions (10.2%). All DCBs used in the study were paclitaxel coated and included the following: SeQuent Please (Braun; Germany), RESTORE (Cardionovum; Germany), Bingo (Yinyi Biotech; China), Swide (Shenqi Medical; China), and Vesselin (Lepu Medical; China).
Adherence was high in the study, with 85.4% and 85.9% of patients in the stepwise and standard DAPT groups, respectively, adhering to their allocated regimens. Due to dyspnea, 7.8% and 9.4% of patients replaced ticagrelor with clopidogrel. Notably, the researchers saw decreased compliance in the handful of days following the switches in protocol at both 1 and 6 months in the stepwise group.
The researchers used an app to contact participants monthly to assess their health status and monitor compliance. Follow-up data were available in 99.3% of patients at 1 year.
The 1-year rate of the primary composite endpoint of all-cause death, stroke, MI, revascularization, and BARC type 3 or 5 bleeding (NACE) was similar for both the de-escalation and standard DAPT groups (9.0% vs 8.7%) and the between group difference of 0.31% met the noninferiority margin of 3.2% (P = 0.013 for noninferiority).
A win-ratio analysis of the secondary endpoint of clinically relevant ischemic or bleeding events (all-cause death, stroke, MI, revascularization, and BARC 2 or 3 bleeding) showed a benefit for stepwise de-escalation of DAPT (win ratio 1.43; P = 0.004). Additionally, BARC type 3 or 5 bleeding was lower in the de-escalation group compared with standard DAPT (0.4% vs 1.7%; P = 0.007). Results remained significant in the per-protocol analysis as well.
Subgroup analyses showed that only patients at high bleeding risk significantly benefitted from standard DAPT compared with those not at high bleeding risk (HR 0.61; 95% 0.35-1.08; P for interaction = 0.039).
‘Probably a Safe Strategy’
Based on the evidence, Gao told TCTMD, he would “strongly recommend” this stepwise de-escalation DAPT strategy for DCB patients at high bleeding risk. “For the rest of patients, I think the physician can decide what's the best for individual patients, he added.
Nieves Gonzalo, MD (Hospital Clinico San Carlos, Madrid, Spain), commenting during a press conference, agreed. “I think what this study shows is that in this specific type of patients that they included [it] is probably a safe strategy,” she said.
Cuisset, too, said the data are “aligned with the evidence with DES that we had before. Probably it means that in some select ACS patient, we can do de-escalation regardless of the PCI strategy, which could be either DES or DCB.”
Further randomized data in this field, specifically the ongoing SELUTION DeNovo study, should help solidify the best treatment plan for these patients, Byrne said. “If that shows promise, then the question around duration of dual antiplatelet therapy after DCB will come more and more into focus,” he said. “So I think it would be good to have more studies, and until then, as a community, I think we have to adopt similar strategies to what we do in patients who have DES.”
Feasibility will be key, however, when planning a DAPT program for patients, and the two regimen changes used here might lead to decreased compliance, Byrne noted. “It's not a strategy I would have chosen to test in a trial, because there's some jeopardy in a double switch,” he said. “You have to think about how easy it is to implement with referring doctors [and] with family practitioners.”
Kirtane agreed. “It almost needs to be programmatically done that way where people realize once they're dropping something that they may need to add something back,” he said, adding that the dose of ticagrelor can also be lowered to de-escalate it. “If you go from 90 BID to 60 BID, that's about the potency of clopidogrel, so that might also be a reasonable strategy.”
Going forward, Kirtane said comparative trials of DAPT strategies in DCB-only patients are not necessary, even though extra evidence is always welcome. “After a study like this, you can say: is it a month? Is it 2 weeks? What agent do we need to use? I certainly think interventionalists would feel that DCB offer a DAPT-related advantage in terms of the minimum duration necessary, and that's a good thing. For a stent, it's typically a month,” he explained.
Worth remembering, said Gao, is that this trial is “not trying to sell or promote DCB to use in all ACS patients. That's a very important message. DCB should be only used in patients who have a suitable indication, for instance ISR, high bleeding risk, or bifurcation. It has to be indicated.”
Yael L. Maxwell is Senior Medical Journalist for TCTMD and Section Editor of TCTMD's Fellows Forum. She served as the inaugural…
Read Full BioSources
Tao L. Stepwise dual antiplatelet therapy de-escalation in patients after drug-coated balloon angioplasty (REC-CAGEFREE II trial). Presented at: EuroPCR 2024. May 15, 2024. Paris, France.
Disclosures
- Tao, Gao, and Cuisset report no relevant conflicts of interest.
- Byrne reports receiving grants/research funding from Abbott, Biosensors International, Boston Scientific, and Translumina.
- Kirtane reports institutional funding to Columbia and/or Cardiovascular Research Foundation from Medtronic, Boston Scientific, Abbott Vascular, Amgen, CathWorks, CSI, Philips, Recor Medical, Neurotronic, Biotronik, Chiesi, Bolt Medical, Magenta Medical, Canon, SoniVie, and Shockwave Medical. He reports personal fees from Amgen, Medtronic, Biotronik, Boston Scientific, Abbott Vascular, CathWorks, Concept Medical, Edwards, CSI, Novartis, Philips, Abiomed, Recor Medical, Chiesi, Zoll, Shockwave, and Regeneron.
- Gonzalo reports receiving grants/research funding from Abbott and honoraria/consulting fees from Abbott, Abiomed, Boston Scientific, Philips, and Shockwave Medical.






Comments