Stroke Thrombectomy Doesn’t Help for Blockages in Smaller Vessels
Three trials showed no improvement in functional outcomes, and the potential for harm, versus medical therapy alone.

Thrombectomy does not improve outcomes among patients with acute ischemic strokes caused by blockages in the medium or distal vessels, results of three randomized trials indicate.
Adding endovascular therapy to best medical therapy or usual care did not boost functional outcomes at 90 days in the DISTAL, ESCAPE-MeVO or DISCOUNT trials, with risks of mortality and symptomatic intracranial hemorrhage that were either similar or higher with the additional procedure.
Not only did DISTAL and the other trials show that endovascular therapy did not provide a benefit, but also they demonstrate that only about half of patients achieve a good functional outcome at 90 days, irrespective of treatment strategy.
“The rest of these people with these smaller strokes remained severely disabled or died, and this is not as good as we would have expected,” DISTAL investigator Urs Fischer, MD (University Hospital Bern, Switzerland), told TCTMD. “We need, in the future, new therapies in order to improve the outcome of these patients.”
The impact of thrombectomy in patients with occlusions in the medium or smaller distal vessels contrasts with strokes caused by large-vessel occlusions (LVOs). In that setting, the mechanical removal of clots has been shown to improve functional outcomes over medical therapy alone in several trials, even among patients with large-core strokes and those presenting late.
Though there had been some nonrandomized data to suggest that thrombectomy would also benefit patients with blockages in the smaller and more distal vessels, these trials dispute that idea.
All three were reported at the International Stroke Conference in Los Angeles, CA, with the results of DISTAL and ESCAPE-MeVO being simultaneously published in the New England Journal of Medicine.
We need, in the future, new therapies in order to improve the outcome of these patients. Urs Fischer
In an NEJM editorial addressing the DISTAL and ESCAPE-MeVO trials, J Mocco, MD (Icahn School of Medicine at Mount Sinai, New York, NY), notes that in recent years, thrombectomy has become more accepted for non-LVO strokes, as reflected in the increasing number of papers on the topic in the literature.
Now, “with high-quality data from randomized, controlled trials in hand, we must critically and cautiously reexamine current practice,” he says, adding, “No matter how one considers these data, there is no question that they represent the current ground zero of evidence to inform decision-making regarding the use of thrombectomy for stroke due to medium- and distal-vessel occlusion. The data clearly show that thrombectomy for distal-vessel occlusions should not be an assumed default care pathway.”
DISTAL
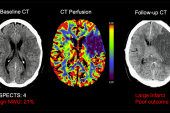
The DISTAL trial, presented by Fischer and Marios Psychogios, MD (University Hospital Basel, Switzerland), included 543 patients (median age 77 years; 44% women) who had an acute ischemic stroke caused by an isolated occlusion in the medium or distal vessels and presented within 24 hours of when they were last known to be well. The median NIHSS score at admission was 6.
Patients were randomized to endovascular therapy plus best medical treatment or best medical treatment alone; 65.4% received IV thrombolysis.
The primary outcome was the level of disability at 90 days, measured using the modified Rankin Scale (mRS) score. There was no significant difference between trial arms in the distribution of mRS scores at that time point (common OR for improvement in mRS score 0.90; 95% CI 0.67-1.22). No benefit was observed in the various subgroups.
Safety did not significantly differ between groups, although there were numerically higher rates of all-cause mortality at 90 days (15.5% vs 14.0%) and symptomatic intracranial hemorrhage within 24 hours (5.9% vs 2.6%) in the thrombectomy arm.
Psychogios told TCTMD the results likely will not stop the use of endovascular treatment in all patients with occlusions in medium or distal vessels, “but I really think that we have to be more selective about the groups of people that we treat with those endovascular means.”
ESCAPE-MeVO
Michael Hill, MD, and Mayank Goyal, MD, PhD (Foothills Medical Centre and University of Calgary, Canada), presented the results of the ESCAPE-MeVO, which was conducted in Canada, the United States, the United Kingdom, Germany, and Hungary. The investigators randomized 530 patients (median age 75 years; 46% women) who had medium-vessel occlusions, presented within 12 hours of when they were last known to be well, and had favorable baseline brain imaging to thrombectomy plus usual care or usual care alone.
The median NIHSS score at baseline was 8 in the thrombectomy group and 7 in the control group. IV thrombolysis was administered in 56.5% and 60.2%, respectively.
The primary outcome was the proportion of patients with an excellent functional outcome (mRS score 0-1) at 90 days, which was 41.6% in the thrombectomy arm and 43.1% in the control arm (adjusted rate ratio 0.95; 95% CI 0.79-1.15). The median mRS score at that time point was 2 in both groups.
None of the secondary outcomes favored thrombectomy. In terms of safety, the procedure was associated with higher rates of 90-day mortality (13.3% vs 8.4%) and symptomatic intracranial hemorrhage (5.4% vs 2.2%).
During his presentation, Goyal noted that there are still many unanswered questions about the use of thrombectomy in medium-sized vessels, including around collateralization of the arteries, speed of treatment, workflow limitations, greater use of general anesthesia, quality of recanalization, the complexity of getting to the correct area, and mRS as an outcome measure. In addition, it’s possible there are certain subgroups of patients who would be more likely to benefit from the procedure, he suggested.
DISCOUNT
In introducing the DISCOUNT trial, Frédéric Clarençon, MD, PhD (Hôpitaux Universitaires Pitié Salpêtrière, Paris, France), noted that distal occlusions represent about 10% to 15% of all acute ischemic strokes. Although the tools exist to perform thrombectomy in these cases, distal vessels are more tortuous, mobile, and fragile than elsewhere, increasing risks of perforation and hemorrhagic complications.
He reported on an interim analysis of the first 163 patients (of a planned 488) who were enrolled in DISCOUNT, which was conducted at 22 French centers. These patients (median age 73.7 years; 47% women) had an acute ischemic stroke involving a distal-vessel occlusion in the anterior or posterior circulation that was confirmed on CT angiography or MRI and who presented within 8 hours of symptom onset (or within 24 hours if there was no hyperintense signal on FLAIR acquisition).
The median NIHSS score at the start of the study was 8. Most (71%) received IV thrombolysis. Thrombectomy was performed using a variety of stent retrievers or aspiration catheters.
The primary outcome was the proportion of patients with an mRS score of 2 or less at 90 days, with those undergoing thrombectomy faring worse than those who received best medical treatment alone (60% vs 77%). Although the odds ratio indicated a lower likelihood of achieving this outcome in the thrombectomy arm (OR 0.42; 95% CI 0.20-0.88), the difference fell shy of the standard for statistical significance in an interim analysis.
Safety was poorer in the thrombectomy arm, with a higher rate of any adverse event (94% vs 81%), any intracranial hemorrhage (44% vs 29%), serious adverse events (39% vs 31%), and symptomatic intracranial hemorrhage (12% vs 6%); the death rate, however, was lower than in the control arm (3% vs 7%).
The trial’s data and safety monitoring board recommended stopping the trial based on these results. Clarençon said the analysis of the overall population is ongoing.
More Work Ahead
Fischer said that a pooled analysis of these trials will be needed to determine whether any subgroups of patients with medium- or distal-vessel occlusions might benefit from thrombectomy since each individual trial was underpowered to answer that question.
There might also be a need for improved devices, Psychogios indicated. “Maybe this also shows that the tools that we have at the moment are not the ones that can help in those situations,” he said. “Maybe we have to get even better tools or use a newer generation than we have available today and design new trials” to achieve better outcomes.
Moving forward, Mocco adds, “further effort, grounded in high-quality data science, is needed to evaluate alternative approaches for medium- or distal-vessel occlusion, be they medical or procedural.”
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Psychogios M, Brehm A, Ribo M, et al. Endovascular treatment for stroke due to occlusion of medium or distal vessels. N Engl J Med. 2025;Epub ahead of print.
Goyal M, Ospel JM, Ganesh A, et al. Endovascular treatment of stroke due to medium-vessel occlusion. N Engl J Med. 2025;Epub ahead of print.
Clarençon F. Mechanical thrombectomy in acute ischemic stroke related to a distal arterial occlusion: interim analysis of the DISCOUNT randomized controlled trial. Presented at: ISC 2025. February 5, 2025. Los Angeles, CA.
Mocco J. Medium- and distal-vessel occlusion—the limit of thrombectomy? N Engl J Med. 2025;Epub ahead of print.
Disclosures
- DISTAL was funded by the Swiss National Science Foundation and others.
- Psychogios reports grants from the Swiss National Science Foundation for the DISTAL, ICARUS, and TECNO trials; a grant from Bangerter-Rhyner Stiftung for the DISTAL trial; unrestricted grants for the DISTAL trial from Stryker Neurovascular, Medtronic, phenox, Penumbra, and Rapid Medical; an unrestricted grant for the ICARUS trial from Acandis; and speaking fees from Stryker Neurovascular, Medtronic, Penumbra, Acandis, and phenox. He is a principal investigator (PI) for the SPINNERS trial, funded by a Siemens Healthineers AG Grant.
- Fischer reports receiving grants the Swiss National Science Foundation and the Swiss Heart Foundation; serving as PI of the ELAN trial and co-PI of the DISTAL, TECNO, SWIFT DIRECT, SWITCH, ELAPSE, and ICARUS trials; receiving research grants from Medtronic, Stryker, Rapid Medical, Penumbra, Medtronic, phenox, and Boehringer Ingelheim; receiving support from the Horton Foundation for the DO IT trial; consulting for Medtronic, with fees paid to his institution; participating in advisory boards for AstraZeneca (former Alexion/Portola), Bayer, Boehringer Ingelheim, Biogen, AbbVie, and Siemens (with fees paid to institution); serving as a member of the clinical event committee for the COATING study (phenox); serving as a member of the data and safety monitoring committee for the TITAN, LATE_MT, IN EXTREMIS, and RapidPulse trials; and being president of the Swiss Neurological Society and president-elect of the European Stroke Organisation.
- ESCAPE-MeVO was supported by grants to the University of Calgary from the Canadian Institutes of Health Research and Medtronic.
- Goyal reports receiving grants/contracts through his institution from Johnson & Johnson Health Care Systems and Medtronic; consulting for Medtronic, Mentice, MicroVention, and Philips; and having a patent involving intracranial access systems, with interest held by MG Stroke Analytics Inc.
- Hill reports receiving stock options from Basking Bioscience; receiving grants/contracts from Boehringer Ingelheim, the Canadian Institutes of Health Research, Medtronic, MicroVention, and NoNO; and consulting for Brainsgate and Diamedica.
- DISCOUNT was funded by the French Ministry of Health and supported by Cerenovus, Balt, Stryker, phenox, MiVi, and Penumbra.
- Clarençon reports giving paid lectures for Balt, Penumbra, Stryker, and Cerenovus; consulting for Balt, Medtronic, Stryker, and MicroVention; being a board member for Artedrone; having stock options with Intradys and LetsGetProof; and serving in a core lab for ClinSearch.




Comments