Subcutaneous ICD Holds Up Well Against Transvenous Devices
PRAETORIAN is the first randomized trial of the therapy, while UNTOUCHED suggests newer iterations are improving outcomes.
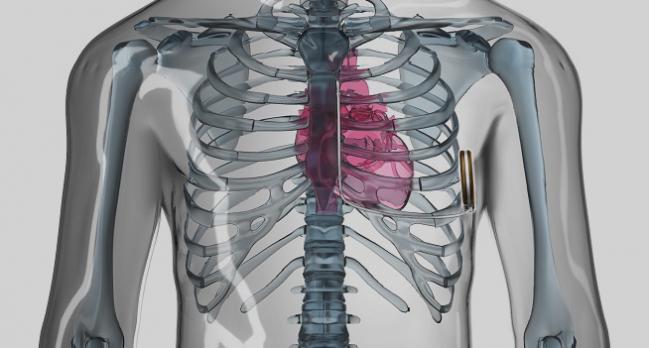
In a typical population of patients requiring implantable cardioverter-defibrillator (ICD) therapy without pacing, mostly for the primary prevention of sudden cardiac death, a subcutaneous ICD (S-ICD; Boston Scientific) provides noninferior results compared with transvenous devices, the randomized PRAETORIAN trial shows. Moreover, results from the single-arm UNTOUCHED study suggest results have gotten better with newer-generation S-ICD technology.
Though inappropriate shocks were more frequent with the S-ICD and overall complications were more common with transvenous devices, neither difference was statistically significant. Lead-related complications, however, were significantly decreased in the S-ICD arm (1.4% vs 6.6%; HR 0.24; 95% CI 0.10-0.54).
“The S-ICD should be considered in all patients in need of an ICD without a pacing indication,” Knops concluded. He noted during a press briefing that since its introduction several years ago, the S-ICD has been mostly a “niche device” for younger patients and others who are expected to need very long-term ICD therapy. “I think that the PRAETORIAN trial now really shows that in the conventional ICD population . . . the S-ICD is a really good alternative option,” Knops said.
The findings are due to be published in the New England Journal of Medicine.
First Randomized Trial of ICD Types
Transvenous ICDs have been shown to effectively reduce the occurrence of sudden cardiac death, but a major limitation is lead failure, which can occur at a rate of 10% to 20% within 6 years, according to Knops. Subcutaneous ICDs were designed to avoid those lead problems. In registry studies of mostly younger patients with preserved LV function, the S-ICD has been shown to have a high shock efficacy, with fewer ICD-related complications but more inappropriate shocks compared with transvenous devices, Knops said.
PRAETORIAN, conducted at 39 centers in Europe and the United States, is the first randomized trial designed to compare the two types of ICDs. Between March 2011 and January 2017, investigators enrolled 849 patients (median age 63 years; 19.7% women) who had a class I or IIa indication for ICD therapy for either primary or secondary prevention and no need for pacing. Overall, 69% had ischemic cardiomyopathy, 23% nonischemic cardiomyopathy, and the rest some “other” condition. Median ejection fraction was 30%. The ICD was for secondary prevention in 19.3% of patients.
Through a median follow-up of 4 years, the S-ICD was shown to be noninferior to transvenous devices in terms of a composite of inappropriate shocks or ICD-related complications that required interventions. There were no significant differences between the subcutaneous and transvenous groups for inappropriate shocks (9.7% vs 7.3%; HR 1.43; 95% CI 0.89-2.30) or overall ICD-related complications (5.9% vs 9.8%; HR 0.69; 95% CI 0.44-1.09).
The main drivers of inappropriate shocks were A-fib/supraventricular tachycardia in the transvenous arm and cardiac oversensing in the S-ICD arm. In terms of complications, a higher number of infections with transvenous devices was counterbalanced by more bleeding with the S-ICD, Knops said.
All-cause death was numerically, but not significantly, more frequent in the patients who received the S-ICD (16.4% vs 13.1%; HR 1.23; 95% CI 0.89-1.70). The number of sudden cardiac deaths in each group was 18, but there tended to be more noncardiovascular deaths in the S-ICD arm. In a chat accompanying the online presentation, a PRAETORIAN investigator said: “We presume that the numerical difference in noncardiovascular death is due to the play of chance.”
UNTOUCHED
During his presentation of the UNTOUCHED results, Michael Gold, MD, PhD (Medical University of South Carolina, Charleston), noted that the most common indication for ICD therapy is primary prevention of sudden cardiac death in patients with an LVEF of 35% or lower, a population that has been underrepresented in prior S-ICD studies. No prospective studies, he said, have examined the S-ICD using contemporary devices and programming in such a population.
UNTOUCHED, conducted at 110 sites, included patients with LV dysfunction (mean LVEF 26%) who required an ICD for sudden cardiac death and did not have a pacing indication. The analysis included 1,111 successful implantations of an S-ICD. Mean patient age was 56, and 25.7% of participants were women. Most patients (53.8%) had ischemic etiology, and 88% had NYHA class II/III heart failure. This population was sicker compared with prior S-ICD studies but comparable—except for a younger age—to participants of landmark transvenous ICD studies, Gold said.
The primary endpoint was freedom from inappropriate shocks through 18 months of follow-up. The observed rate was 95.9%, exceeding the performance goal of 91.6% derived from the high-rate and long-duration arms of the MADIT-RIT trial (P < 0.0001).
The 1-year rate of inappropriate shocks in the overall cohort was 3.1%, reaching 2.4% in those with the latest-generation device. That’s the lowest rate seen in an S-ICD study and lower than in many transvenous ICD trials, Gold said.
The study also demonstrated an all-cause shock-free rate of 90.6% at 18 months, exceeding the performance goal of 85.8% (P < 0.0001).
There were 64 appropriate shocks during the study, and the S-ICD provided a 92.2% first shock success rate and 98.4% final shock success rate. The one episode associated with a failed final shock converted spontaneously, Gold reported. In addition, there was a 100% final conversion rate for all ventricular tachycardia storm events.
Overall survival was 94.9% at 18 months. Of the 53 deaths, there were three related to arrhythmia (two pulseless electrical activity and one asystole).
“The UNTOUCHED study shows high S-ICD efficacy and safety with contemporary devices and programming despite the sickest cohort studied to date,” Gold concluded.
The study is “very important,” according to David Callans, MD (University of Pennsylvania, Philadelphia), who provided commentary after Gold’s presentation. It “successfully demonstrated in a large population of patients a remarkable reduction in inappropriate shock incidence with improvement in technology and programming,” he said.
Moreover, Usha Tedrow, MD (Brigham and Women’s Hospital, Boston, MA), who provided additional perspectives, said UNTOUCHED “provides some important corroborating evidence that adding specialized high-pass filtering can further improve the inappropriate shock rate for the S-ICD.” In the study, use of the SMART Pass filter was associated with a reduction in inappropriate shocks.
Who Should Get a Subcutaneous ICD?
Speaking after Knops’ presentation, Sana Al-Khatib, MD (Duke University Medical Center, Durham, NC), welcomed the randomized data and pointed out that even though the S-ICD was associated with fewer complications and more inappropriate shocks, the trial was not powered for those endpoints separately.
She indicated that the choice of ICD should be discussed with patients. “In the majority of patients with ICD indications who don’t need to pace and who pass the screening test, the option of an S-ICD versus a transvenous ICD should be presented to the patient,” she said. “However, I personally would not extrapolate the results of the PRAETORIAN trial to every patient we see in clinical practice and I’m really intrigued by the role of the S-ICD in patients with [hypertrophic cardiomyopathy], who are known to be at a higher risk of inappropriate shocks.”
Eric Prystowsky, MD (Ascension Medical Group, Indianapolis, IN), also commenting on the PRAETORIAN results, urged some caution in interpretation. He said the secondary prevention population was too small for the results to apply in that setting, adding similar concerns for the hypertrophic cardiomyopathy subgroup. “They can be a problem with sensing with the subcutaneous device, so I’d be a little careful looking there,” advised.
Prystowsky also said he was “a little disturbed” by the rate of inappropriate shocks in the transvenous arm: “There are lots of ways to avoid inappropriate shocks, and I think 6% is way too high in the modern era.”
Assuming that S-ICD and transvenous devices are “equal as far as problems are concerned,” clinicians then have to decide who should get what type of ICD, he said. Two things to consider, he added, are cost—in the US, the S-ICD “is significantly more expensive”—and battery life. “In some of the transvenous ICDs now, the battery life is quite long and certainly is going to outlast the subcutaneous ICD,” Prystowsky said.
But he indicated that there could be role for the S-ICD. “I think it boils down to: [in] a primary prevention patient who doesn’t need pacing, who you don’t think is going to need [cardiac resynchronization therapy], and who you feel that maybe it’s okay to go ahead and use it and you’re not worried about the money or the longevity, I’d say take your pick.”
Photo Credit: Boston Scientific. ©2020 Boston Scientific Corporation or its affiliates. All rights reserved.
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Knops RE. PRAETORIAN: a prospective, randomized comparison of subcutaneous and transvenous implantable cardioverter-defibrillator therapy. Presented on: May 8, 2020. HRS 2020.
Gold M. Understanding outcomes with the S-ICD in primary prevention patients with low ejection fraction (UNTOUCHED) trial primary results. Presented on: May 8, 2020. HRS 2020.
Disclosures
- PRAETORIAN was funded by Boston Scientific.
- UNTOUCHED was sponsored by Boston Scientific.
- Knops reports receiving consultancy fees and research grants from Abbott, Boston Scientific, Cairdac, and Medtronic, as well as having stock options from AtaCor Medical.
- Gold reports conducting clinical trials for and receiving consulting fees from Boston Scientific and Medtronic.


Comments