SURTAVI Lends More Support to Use of TAVR in Intermediate-Risk Patients
(UPDATED) Combined with PARTNER 2A, the trial supports strengthening a guideline recommendation that is just days old, multiple experts say.
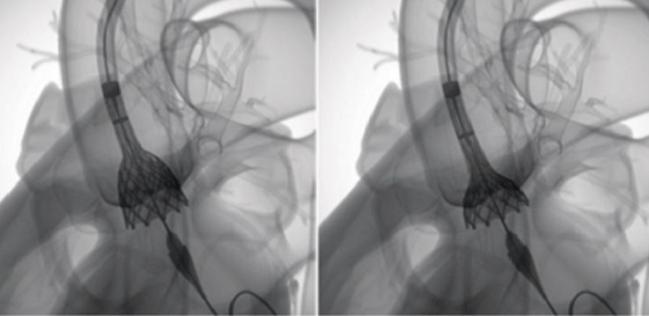
WASHINGTON, DC (UPDATED)—Another trial, this time using self-expanding bioprostheses, has shown that TAVR is noninferior to surgical valve replacement in patients with symptomatic severe aortic stenosis and an intermediate surgical risk, leading some to call for the upgrade of a guideline recommendation that came out just this week.
In SURTAVI, the 2-year rate of all-cause death or disabling stroke was 12.6% in patients who underwent TAVR with either the first-generation CoreValve prosthesis or next-generation Evolut R (both Medtronic) and 14.0% with surgery, a difference that met criteria for noninferiority, Michael Reardon, MD (Houston Methodist DeBakey Heart and Vascular Center, TX), reported at the American College of Cardiology 2017 Scientific Session here.
The results, which were published simultaneously online in the New England Journal of Medicine, join those from PARTNER 2A in showing that TAVR with either self-expanding or balloon-expandable valves is at least as good as surgery in patients with intermediate risk.
The PARTNER 2A results led to a change this week in the guidelines for valvular heart disease, which now contain a class IIa recommendation stating that TAVR is a reasonable alternative to surgery in the intermediate-risk population.
Reardon said that based on the “outstanding data” from SURTAVI, that newly minted guidance should be strengthened, and other experts, including Gregg Stone, MD (NewYork-Presbyterian/Columbia University Medical Center, New York, NY), agreed.
“I would make it a class I indication,” he told TCTMD. “You now have two very large, well-done studies that show—at least with relatively short-term follow-up—that transcatheter aortic valve replacement is associated with lower morbidity and outcomes in terms of death and stroke at least as good as with surgical aortic valve replacement.”
An important issue in patients with intermediate risk, who are expected to have relatively long survival, is how durable the results of TAVR will be over the long term, he added.
“I think it’s not unreasonable to consider that both [surgical AVR] and TAVR would be class I, and patients should be informed about the differing risk profiles of the two approaches and certainly about the unknown long-term durability of TAVR before they make a decision,” Stone said.
But not everyone agreed that a class I indication is warranted at this point.
The results of SURTAVI and PARTNER 2A “support use of TAVR in some, but not all, intermediate-risk patients; specifically, TAVR is appropriate only if a bioprosthetic valve is preferred over a mechanical valve and if long-term valve durability (greater than 10 years) is not a concern in that individual patient,” Catherine Otto, MD (University of Washington, Seattle), who co-chaired the guideline writing group, told TCTMD in an email.
The updated guidelines from the American Heart Association/American College of Cardiology, along with rapid recommendations that came out last year, “provide comprehensive evidence-based recommendations for this decision-making process,” Otto continued. “The SURTAVI trial adds support to those recommendations but does not change them.”
Regarding the need to strengthen the recommendation to class I, John Erwin III, MD (Texas A&M College of Medicine/Baylor Scott & White Health, Temple, TX), a member of the guideline writing group with Otto, told TCTMD in an email that he “would not rebut those opinions too strongly.” But, he added, “we must keep in mind both the body of data that we have in the long term for [surgery], as well as our concerns about the outcomes of patients with significant residual regurgitation and a need for permanent pacing and the niggling concern about long-term durability with TAVR.”
He pointed out that the difference between a class I and class IIa recommendation is the use of “is recommended” rather than “is reasonable.” Taking that and unanswered questions into consideration, Erwin said, “I think it is reasonable for it to remain class IIa until we have longer-term follow up of these patients.”
Procedure-Related Complications Differ
SURTAVI randomized 1,746 patients at 87 centers in the United States, Europe, and Canada; 1,660 underwent an attempted TAVR or surgery. All were considered by their local heart teams to have an intermediate surgical risk, with an average STS PROM score of 4.5%.
The first-generation CoreValve bioprosthesis was used in 84% of patients in the TAVR arm, with Evolut R used in the rest. Transfemoral access was used in 94%, with a minority undergoing direct aortic (4%) or subclavian (2%) procedures. Embolic protection was not allowed.
The noninferiority of TAVR for the primary composite endpoint of all-cause death or disabling stroke at 2 years was established using a novel Bayesian statistical method that combined observed event rates among patients who had reached 2 years of follow-up and imputed data from those who had not yet been followed for that long. That allowed study investigators to release the results more rapidly, Reardon said.
He highlighted the mortality findings in both the TAVR and surgery arms of the trial. At 30 days, the mortality rate following surgery was just 1.7%, which Reardon called “extraordinary.” Despite such good results, TAVR still matched up throughout study follow-up.
At 2 years, the all-cause mortality rate was 11.4% with TAVR and 11.6% with surgery. Those rates are lower compared with prior TAVR trials, which can be attributed to the lower-risk population enrolled in SURTAVI, Reardon said.
The rate of disabling stroke through 2 years did not differ significantly between arms, although there was a trend favoring TAVR (2.6% vs 4.5%).
Procedure-related complications differed between trial arms. Surgery was associated with higher rates of acute kidney injury stage 2 or 3 (4.4% vs 1.7%), new or worsening A-fib (43.4% vs 12.9%), and transfusion, and TAVR was associated with elevated rates of major vascular complications (6.0% vs 1.1%) and pacemaker implantation (25.9% vs 6.6%).
Reardon touted the hemodynamic findings achieved with TAVR. Although patients in both trial arms had improvements, TAVR resulted in lower mean gradients and large aortic valve areas, “findings that probably stemmed from the supraannular design of the self-expanding bioprosthesis,” Reardon et al note.
Moderate or severe residual paravalvular regurgitation at 1 year was more common following TAVR, however (5.3% vs 0.6%). That’s not surprising, Reardon said, pointing out that most valves used in the TAVR arm were first generation.
Among other secondary outcomes, there were more reinterventions and hospitalizations following TAVR. There were gains in functional class and quality of life in both groups, although both measures favored TAVR at 1 month, indicating more rapid improvement.
No structural valve deterioration was seen in either group during follow-up.
Stone said the study “shows clear noninferiority” of TAVR versus surgery, but he added that because of differences in complications and echocardiographic findings between trial arms, “very long-term follow-up is going to be required to see if there’s any differences in terms of long-term valve integrity or structural deterioration.”
A Worthy Competitor, but Questions Remain
In a panel discussion following Reardon’s presentation, David Cohen, MD (Saint Luke’s Mid America Heart Institute, Kansas City, MO), said SURTAVI shows that TAVR is a worthy competitor when matched against surgery, results in more rapid quality-of-life improvements, and carries a lower stroke risk.
“I don’t think that’s a fluke at this point,” he said about the stroke finding, pointing out that other studies have shown similar significant or nonsignificant differences. “I think that’s a real benefit.”
There are, however, some unresolved questions, Cohen said. For one, it remains unclear whether the hemodynamic advantages of TAVR carry any advantages in terms of outcomes over longer-term follow-up. And secondly, the high pacemaker rate is a concern in a group of patients who are expected to live an average of 12 years.
Reardon said he and his co-investigators were somewhat surprised by the pacemaker rate because there are data to suggest that Evolut R carries a lower rate than the first-generation CoreValve. He indicated that the high rate could have to do with how the devices were implanted and noted that some of the trial centers were new to implanting the newer device when it was introduced.
Martin Leon, MD (NewYork-Presbyterian/Columbia University Medical Center), who was co-principal investigator for PARTNER 2, said the implications of the higher pacemaker rate with TAVR are debatable, “but as you get into lower-risk candidates, certainly what you don’t want to do is commit one in four patients to having a permanent pacemaker at a young age.”
Another potential concern, Erwin said, is the higher rate of paravalvular regurgitation with TAVR. “Previous studies have shown that moderate-to-severe paravalvular regurgitation is associated with higher rates of morbidity and mortality, and we will need longer-term follow-up to see how that group of patients fares,” he said.
Leon pointed out that TAVR has always been associated with a higher rate of paravalvular regurgitation versus surgery and that the problem is improving with each new generation of devices.
“We’re getting down to low enough paravalvular leak rates where the differences are really not so meaningful and appear not to have an important impact on the key clinical outcomes, which are really death and stroke,” he said. He agreed with Reardon and Stone that SURTAVI and PARTNER 2A combined should strengthen the recommendation for TAVR in intermediate-risk patients to class I.
Photo Credit: Medtronic (adapted with permission from http://www.corevalve.com/evolut-r/product/index.htm)
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Reardon MJ, Van Mieghem NM, Popma JJ, et al. Surgical or transcatheter aortic-valve replacement in intermediate-risk patients. N Engl J Med. 2017;Epub ahead of print.
Disclosures
- SURTAVI was funded by Medtronic.
- Reardon reports receiving consulting fees paid to his institution from Medtronic.
- Stone reports no relevant conflicts of interest.


Comments