TCT 2019 Day Four: Costs and Quality of Life Take Center Stage
Last day of TCT 2019! Here’s what we’re watching.

SAN FRANCISCO, CA—It’s the last day of TCT 2019 and all of us on the TCTMD news team have our eyes on the finish line. But first, the late breakers.
Leading off the late-breaking clinical trials was Suzanne J. Baron, MD (Lahey Hospital and Medical Center, Burlington, MA), presenting a cost-efficacy analysis from COAPT. As Baron showed this morning, follow-up costs are significantly lower following MitraClip implantation than in the optimal medical therapy group, but the upfront costs of the device as well as of the hospital mean that the cumulative 2-year costs outstrip those of a drug-based strategy.
The cost per quality-adjusted life-year gained, however, falls within the ‘acceptable economic value’ according to established US thresholds, Baron said. And staying alive? That requires money. Even if the device was free, she said, costs would STILL be higher.
“With the cost of these technologists, we’re going to automatically be in the hole once we start,” Baron told me. “The reality is that though we see costs offset, we can’t make all of that cost up and the reason for that is that staying alive is expensive. We actually did a sensitivity analysis that looked to see whether this procedure would be cost-saving if the device itself was free. Even with it costing zero dollars, this procedure still is not cost saving, because people stay alive longer.”
TCTMD's full coverage is HERE.
Dr. @SuzanneJBaron presents ‘COAPT: Cost Effectiveness Analysis From a RCT of the MitraClip in Patients With HF & Severe Secondary MR’! Simultaneous pub in @CircAHA! #TCT2019 @crfheart @NMHheartdoc @GreggWStone @Drroxmehran #AnitaAsgar @sameergafoor pic.twitter.com/EaQQ1JRy7b
— Poonam Velagapudi (@Pooh_Velagapudi) September 29, 2019
****
PARTNER 3 Health Status Outcomes
Baron was back to present health status outcomes from another well-known structural heart trial, this one PARTNER 3. In this analysis, looking at patients with severe aortic stenosis at low surgical risk, both TAVR and SAVR resulted in substantial health status benefits at 12 months despite most patients having NYHA class I or II symptoms at baseline.
In this substudy, Baron and colleagues used the Kansas City Cardiomyopathy Questionnaire (KCCQ) overall summary score (ranging from 0 to 100) to assess health status outcomes through 1 year in both study groups. The mean baseline KCCQ overall summary score was 70 for both TAVR and SAVR patients, which corresponds to NYHA class II symptoms.
Dr. Suzanne Baron presenting PARTNER 3 health status outcomes for low surgical risk patients w severe AS - TAVR v SAVR #TCT2019 pic.twitter.com/i17UOWiBpI
— Angioplasty.Org (@angioplastyorg) September 29, 2019
As expected, TAVR patients demonstrated substantially improved health status at 1 month. However, “in contrast to prior studies,” Baron reported that the benefit of TAVR over surgery persisted through 6 (2.6 point difference; P = 0.002) and 12 months (1.8 point difference; P = 0.03), although the magnitude was smaller. At 1 year, both groups had experienced an improvement of about 19 points from baseline, which is consistent with a large clinical improvement.
“When compared with SAVR, TAVR as associated with significantly improved disease specific health status not only at 1 month, but also at 6 and 12 months,” Baron said.
Durability will be key, however, and Baron’s group will be following this question and its impact on health outcomes beyond the first year.
Full story can be found here.
What a great role model! Congratulations @SuzanneJBaron !! So great to see a woman in the main arena with late breaking studies. #WIN #WISH #CRFWISH #SHD #TCT2019 @Pooh_Velagapudi @Drroxmehran @tiffchenMD @TCTConference https://t.co/54t9pNI7Kt
— Vivian Ng (@DrVivianNg) September 29, 2019
****
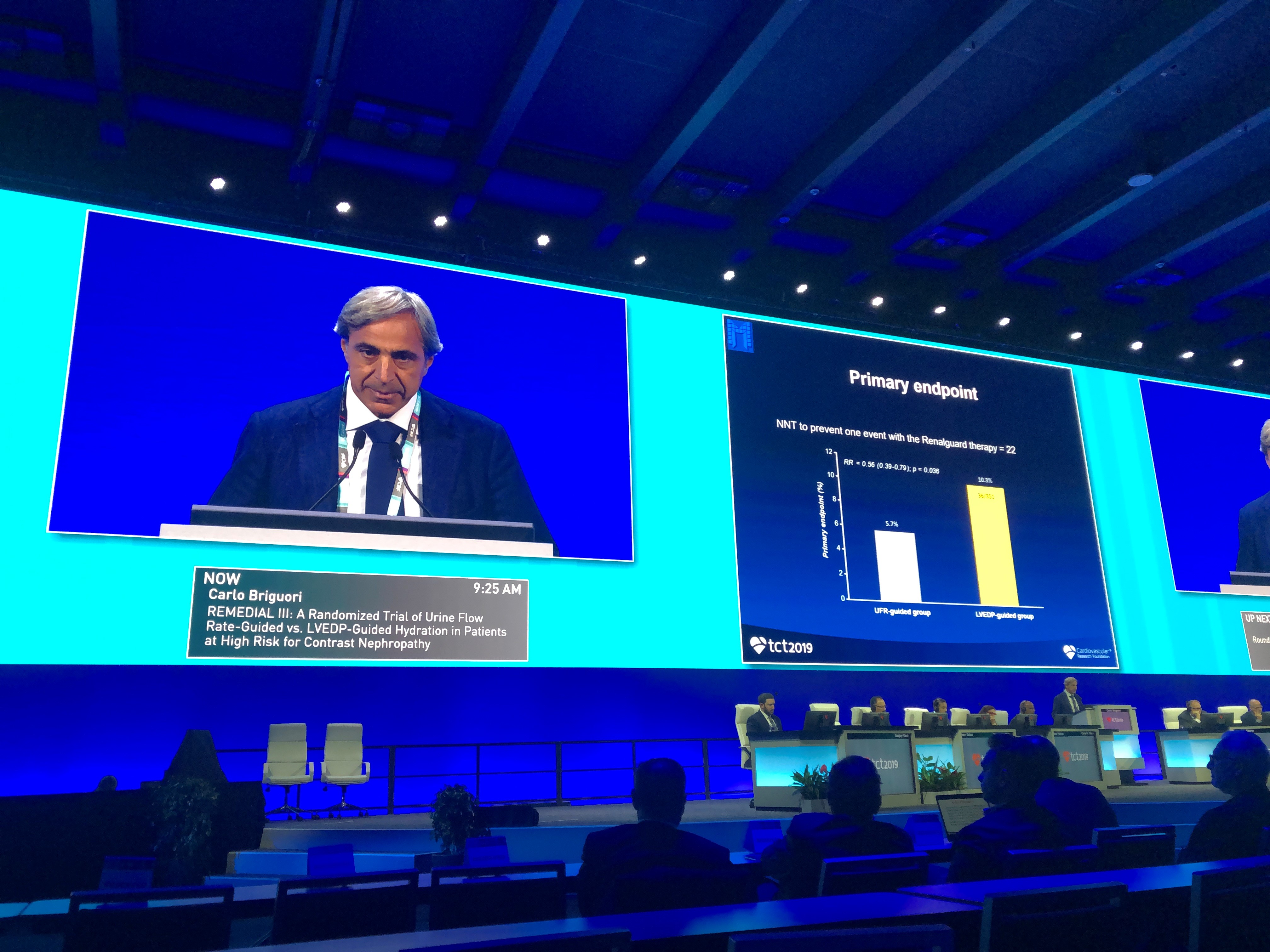 The third and final late-breaker was REMEDIAL. This investigator-initiated randomized trial compared two tailored hydration strategies to prevent contrast-induced acute kidney injury. As Carlo Briguori, MD (Mediterranea Cardiocentro, Naples, Italy), showed here, a strategy guided by urine flow rate (UFR) proved superior to an approach guided by the left ventricular end diastolic pressure (LVEDP).
The third and final late-breaker was REMEDIAL. This investigator-initiated randomized trial compared two tailored hydration strategies to prevent contrast-induced acute kidney injury. As Carlo Briguori, MD (Mediterranea Cardiocentro, Naples, Italy), showed here, a strategy guided by urine flow rate (UFR) proved superior to an approach guided by the left ventricular end diastolic pressure (LVEDP).
Using the UFR-guided approach, the goal with the hydration regimen is to achieve a UFR of 300 mL/hour prior to the intervention and the maintenance of a UFR of more than 450 mL/hour during the procedure. With the UFR-guided strategy, 5.7% of patients developed contrast-induced acute kidney injury and/or pulmonary edema post procedure compared with 10.3% of patients randomized to the LVEDP-guided approach (RR 0.56; 95% CI 0.39-0.79).
Hypokalemia occurred in 6.2% of the patients in the UFR-guided group, a risk that was significantly higher than in those randomized to the LVEDP strategy. As a result, potassium replacement was necessary in more patients in the UFR-guided strategy and investigators recommend a strict control of potassium balance with the UFR-guided approach.
Check back for full results.
*****
That's not quite all for TCT 2019, but they're kicking us out of the convention center here soon! Check back on TCTMD over the next few hours (and days) to get the results from the last late-breakers of the meeting. These are BIODEGRADE, BLADE-PCI, FORZA, and IVUS-XPL: 5-Year Outcomes.
Shelley Wood was the Editor-in-Chief of TCTMD and the Editorial Director at the Cardiovascular Research Foundation (CRF) from October 2015…
Read Full Bio

Comments