Thrombolysis ‘Safe and Effective’ for Obstructive Mechanical Valve Thrombosis
Slow tPA infusion should be offered to “most eligible patients” with obstructive PVT, says editorialist Hartzell V. Schaff.

Administered slowly, low-dose infusions of tissue plasminogen activator (tPA) are associated with low mortality and high treatment success rates in patients with obstructive prosthetic valve thrombosis (PVT) over 3 months and provide a “safe and effective alternative” to surgery, according to a new observational study.
Randomized trials are needed to better guide management of these patients, especially in deciding whether surgery is warranted, the researchers say.
But study co-author Ahmet Güner, MD (Mehmet Akif Ersoy Thoracic and Cardiovascular Surgery Training and Research Hospital, Istanbul, Turkey), in an email to TCTMD, stressed that this analysis, while not randomized, is “unique in this field” in that it prospectively enrolled patients eligible for either treatment at multiple high-volume centers and compared outcomes head-to-head.
Thrombolysis is typically preferred by patients hoping to avoid an invasive reoperation for thrombectomy or replacement, but it has been linked with unacceptable rates of thromboembolism, bleeding, and even death. Because of this, recent studied have aimed to refine tPA administration by showing that a slow (6 hour) or ultraslow (25 hour) infusion without an initial bolus, avoidance of heparin, and echocardiographic surveillance can all increase the chances of success with thrombolytic therapy.
HATTUSHA Results
For the HATTUSHA study, published in the March 15, 2022, issue of the Journal of the American College of Cardiology, Mehmet Özkan, MD (Koşuyolu Kartal Heart Training and Research Hospital, Istanbul, Turkey), and colleagues aimed to provide a contemporary comparison of thrombolysis and surgical outcomes in this patient population.
They enrolled 158 patients with obstructive PVT (65.2% women; median age 49 years) who were treated at one of eight tertiary centers between December 2013 and December 2020. All patients were deemed suitable for both surgery and thrombolytic therapy, and treatment decisions were made with the heart team and the patient.
Among the 52.5% of patients who were treated with thrombolytic therapy—using low-dose tPA (25 mg) given with the slow (6 hours) and/or ultraslow (25 hours) infusion protocols mostly in repeated sessions—the success rate was 90.4% with a median tPA dose of 59 mg. Hospital length of stay was longer and rates of minor and major complications, major bleeding, rethrombosis, and mortality at 3 months (the primary endpoint) were all higher with surgery. Most deaths occurred during the hospital stay, with only one patient in each group dying after hospital discharge.
Adverse Events in Obstructive PVT Patients
|
|
Thrombolytic Therapy |
Surgery |
|
|
(n = 83) |
(n = 75) |
|
3-Month Mortality |
2.4% |
18.7% |
|
Minor Complications |
8.4% |
38.7% |
|
Major Complications |
6.0% |
41.3% |
|
Total Embolic Complications |
2.4% |
5.3% |
|
Major Bleeding |
2.4% |
9.3% |
|
Rethrombosis Requiring Therapy |
2.4% |
6.7% |
|
Median Hospital Stay, days |
5 |
9 |
Within the surgery group, 62.7% experienced complications: 12 bleeds, six cases of embolism or thrombosis, and 76 other events. Only 12% of the patients in the thrombolytic therapy arm reported complications: seven bleeds, five cases of embolism or thrombosis, and two other events.
“Surgery has a high mortality rate even in experienced centers; therefore, thrombolytic therapy may be considered as a beneficial treatment strategy in patients with obstructive prosthetic valve thrombosis in the absence of contraindications,” the authors write.
Controversy Continues
In an accompanying editorial, Hartzell V. Schaff, MD (Mayo Clinic, Rochester, MN), writes that the study “addresses several issues regarding the controversy of initial thrombolytic therapy or reoperation for mechanical valve thrombosis.” Specifically, he points to the previously unknown risk of recurrent thrombosis after successful lysis, which the authors show is just as prevalent, if not more so, with surgery.
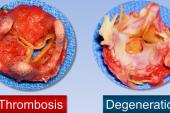
Even if large, randomized trials are conducted in this space going forward, “it is unlikely that such studies will guide medical versus surgical therapy of valve thrombosis in the near future,” Schaff predicts. “Reoperation for valve thrombectomy or replacement will be necessary for patients with cardiogenic shock, patients with associated pannus underlying thrombus formation, as well as patients with contraindications to thrombolysis including left atrial clot.”
But ultimately these data “establish the effectiveness and relative safety of slow and/or ultraslow tPA infusion, which should be offered to most eligible patients with thrombotic obstruction of mechanical valves,” he concludes.
In the paper, Özkan, Güner, and colleagues point out that US and European guidelines are at odds as to how to manage patients with obstructive PVT, with the 2020 American College of Cardiology/American Heart Association guidelines carving out a bigger role for thrombolytic therapy than those of the European Society of Cardiology/European Association for Cardio-Thoracic Surgery 2021 guidelines, which prioritize urgent surgery over fibrinolysis, with the latter only recommend if surgery is not available or considered too high risk.
Güner, acknowledging that their study was not a randomized trial, insisted the results warrant consideration, stressing that patients treated with thrombolytics had fewer complications, shorter hospital stays, and better survival.
“For such rare diseases, guideline committees, and task forces may not necessarily wait for strong evidence coming from [randomized] data, because this may deprive the patients of the novel treatment options,” he said. “Analyzing best available evidence and synthesizing it with expert opinion may serve as the best way to generate recommendation[s].”
Yael L. Maxwell is Senior Medical Journalist for TCTMD and Section Editor of TCTMD's Fellows Forum. She served as the inaugural…
Read Full BioSources
Özkan M, Gündüz S, Güner A, et al. Thrombolysis or surgery in patients with obstructive mechanical valve thrombosis: the multicenter HATTUSHA study. J Am Coll Cardiol. 2022;79:977-989.
Schaff HV. Progress in management of mechanical valve thrombosis. J Am Coll Cardiol. 2022;79:990-992.
Disclosures
- Özkan, Güner, and Schaff report no relevant conflicts of interest.



Comments