Transcatheter Fix for Native Aortic Valve Regurgitation ‘Not Optimal’ but Getting Better
Danny Dvir hopes new registry data will help inform decisions on when and how to treat high-risk NAVR, but new tech is needed.
WASHINGTON, DC—There’s fresh evidence that off-label use of TAVR devices for pure native aortic valve regurgitation (NAVR) is associated with “not optimal” outcomes, although newer-generation devices, particularly repositionable valves, may help.
“Although significant improvement is seen with newer-generation transcatheter heart valve (THV) devices, TAVR for NAVR is a challenging approach associated with limited procedural efficacy,” Danny Dvir, MD (University of Washington Medical Center, Seattle), said here at the CRT 2018 meeting. “Widely utilized THV devices have suboptimal clinical outcomes in native aortic valve replacement, including malposition, significant aortic regurgitation, and a need for a second THV.”
This is the second recent study to try to get a snapshot of the patients undergoing transcatheter valve implantation for NAVR. Late last year, Yoon et al published results of their review of a pure native AR TAVR registry and reached similar conclusions, namely, that newer-generation devices were associated with significantly better outcomes in these patients.
There are currently no transcatheter devices indicated for the treatment of isolated, noncalcified NAVR. One device, the JenaValve, was designed with unique clips that made it amenable to NAVR, Dvir explained to TCTMD, and indeed it received CE Mark approval for both aortic stenosis and native, noncalcified aortic insufficiency. That first-generation device, however, has since been removed from European markets. A second-generation device is in the works.
Still, patients turned down for surgery have nevertheless been treated with transcatheter devices over the years. Dvir and colleagues set out to look retrospectively at patient characteristics, treatment, and outcomes among patients with NAVR treated off-label in the VIVID registry.
In all, 254 patients in the registry had been treated for “pure” NAVR at the time investigators “locked” the data to review results in August 2017. Mean age was 74, mean STS score was 6.5, and LVEF was “mildly reduced” at a mean of 45%. Most patients were treated via a transfemoral procedure and the most commonly used device was the CoreValve, in 41% of cases, followed by the Evolut R or Pro (15%). The balloon-expandable Sapien XT and Sapien 3—trickier to anchor in the absence of calcium—were used in the minority of cases (7%) and the remainder were devices not approved in the US. Indeed, several of the valves including the Direct Flow (8%), Engager (4%), along with the JenaValve (13% of procedures), are no longer commercially available.
Mean contrast use was “high,” said Dvir, at 163 ML. General anesthesia was used in 60%, and hospital stays were “long”—12 days on average, including 4 days in the ICU. New pacemaker implantation was nearly 20%.
Early safety was not statistically different between first- and later-generation devices, but beyond 30 days, compared with first-generation devices, newer-generation devices—many of them repositionable—were associated with reduced efficacy. All-cause mortality, cardiac mortality, stroke, valve-related dysfunction, moderate or severe aortic regurgitation, and NYHA class III or IV heart failure were all higher among patients treated with first- versus newer-generation devices.
Efficacy Beyond 30 Days Post-TAVR
|
First-Generation THV (n = 109) |
Newer-Generation THV (n = 145) |
|
|
Clinical Efficacy |
56% |
72% |
|
All-Cause Mortality |
17% |
8% |
|
Cardiac Mortality |
12% |
7% |
|
Noncardiac Mortality |
5% |
1% |
|
All Stroke |
3% |
4% |
|
Valve-Related Dysfunction |
29% |
10% |
|
Moderate or Severe AR |
26% |
5% |
|
NYHA Class III or IV |
18% |
13% |
In additional analyses, significant predictors of mortality included nontransfemoral access, pulmonary hypertension, moderate or greater aortic regurgitation, STS score > 8%, and acute kidney injury of grade 2 or greater.
Those predictors may be one clue to how NAVR patients should be treated going forward, Dvir observed. “Better clinical outcomes could be expected if patients are referred at an earlier clinical stage,” he said during his late-breaking clinical trial presentation. “Novel THV devices, designed to treat native aortic valve regurgitation may improve clinical outcomes, but this needs more clinical attention,” he concluded.
Following his press conference presentation of the data, Dvir was asked if he felt these results should cause physicians to reconsider trying to treat NAVR with the currently available devices.
For Dvir, that’s a step too far, since interventionalists will always feel compelled to help patients who have no other options. “We are physicians, we work in the hospital, we have challenging patients, and we have to decide whether to embark on a procedure associated with not-optimal clinical outcomes,” he said. “What’s needed is a discussion and showing the data and the [shortcomings] of the prosthetic with the patient and with other physicians in the hospital.”
Elaborating later to TCTMD, he took a firmer stance: “We should not stop [treating these patients]. We should continue to learn and understand what are the specific characteristics that lead to the complications. All of this data collection eventually should lead to understanding how we should do the perfect trial, and which what device for that trial.”
The current TAVR devices, for a range of reasons—lack of repositionability, expansion mechanics, imprecise delivery—are not well suited to NAVR, but Dvir is optimistic that “dedicated devices” will emerge down the road.
Commenting on the study for TCTMD, Neil Moat, MD (Royal Brompton Hospital, London, England), had some concerns about the patients being offered transcatheter treatment: mean age 75, relatively low STS scores, and comorbidities that “don’t look that bad.”
As we all know, what you see on a list of comorbidities doesn’t really tell you what the patients were like, Moat said, but these “didn’t look like a particularly extreme risk population.”
“I think you could conclude from that presentation that, wherever possible, these patients should have surgery,” he commented. “Surgery remains the gold standard. If they really are inoperable, then treatment with a recapturable, repositionable device is worth discussing.”
An Evolving Field
In the discussion following Dvir’s late-breaking presentation, Jeffrey Popma, MD (Beth Israel Deaconess Medical Center, Boston, MA), asked whether, in an era of better valve sizing, use of more rapid pacing, and the ability to retrieve/reposition THVs, if “evolution of the procedural technique” can also be credited with improvements in outcomes over time.
Dvir, in response, acknowledged that there is less postprocedural aortic regurgitation than in the past, but said that “the results are still not comparable . . . to conventional [aortic stenosis] patients coming for the procedure. Clearly, the technique has evolved and is continuing to evolve, but I [do] think we need better devices designed specifically for aortic regurgitation.”
Also on the panel, Maurice Buchbinder, MD (Foundation for Cardiovascular Medicine, San Diego, CA), asked whether Dvir and colleagues had evaluated outcomes among patients treated with two THVs. In a handful of cases, Buchbinder said, he and others have adopted “a priori” two-valve approach.
“Take the cost aside—we use the first valve as an anchor, on the low side, and the second one where it should be, and the combination of the two has helped,” he explained.
Dvir, however, pointed out that the aortic regurgitation numbers he presented consider the final outcome. “So even after using two valves, we have poor results,” Dvir said.
An a priori plan of using two valves is expensive, he added, “and not without risks to the coronaries.”
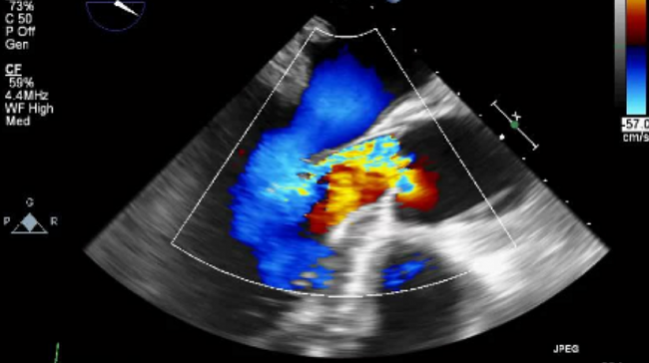
Photo Credit: Adapted from Yin W-H. TAVR for pure native aortic valve regurgitation – a horrifying ride. Presented at: TCT 2017. October 30, 2017. Denver, CO.
Shelley Wood was the Editor-in-Chief of TCTMD and the Editorial Director at the Cardiovascular Research Foundation (CRF) from October 2015…
Read Full BioSources
Dvir D. Transcatheter aortic valve replacement for the treatment of pure native aortic valve regurgitation in selected non-surgical candidates. Presented at: CRT 2018. March 5, 2018. Washington, DC.
Disclosures
- Dvir reports financial arrangements or affiliations with Edwards Lifesciences, Medtronic, Abbott, and Jena Valve.


Comments