Tricuspid Valve Interventions in High-Risk Patients: Midterm Outcomes Encouraging in TriValve Registry
Though it’s early days, a multitude of transcatheter devices as a whole are showing high procedural success, favorable survival, and clinical gains.
Transcatheter valve interventions for severe symptomatic tricuspid regurgitation (TR) produce “favorable” midterm survival despite being done in a high-risk population, according to new numbers from the TriValve Registry.
This data set represents the largest series of tricuspid interventions so far and is notable for including more advanced patients than those typically enrolled in clinical trials, lead author Maurizio Taramasso, MD, PhD (University Hospital of Zurich, Switzerland), told TCTMD. The TriValve results, published online last month in JACC: Cardiovascular Interventions, suggest these high-risk individuals merit further study, he said.
“We are quite far from [knowing] which patients could actually benefit, but still there are patients who definitely could benefit,” he said. “The risk factors we found for better outcome are all risk factors for valve disease, so this tells us we should probably start treating patients a bit earlier.”
Moreover, Taramasso noted, “there are a lot of studies telling us that if you reduce TR just a little bit you can improve the symptoms, even if you don’t have a huge reduction in TR.” With TR as the target, improved patient selection and continued device development are needed, he added. “It’s clear that the more we reduce TR, the better the outcome.”
Even now, these findings should encourage general cardiologists to be on the lookout for patients with tricuspid valve disease, so that they can receive timely care, Taramasso urged.
TriValve Over Time
Taramasso and colleagues looked at data on 312 high-risk patients with severe TR (93% of functional etiology) treated at 18 centers in North America and Europe. More than half (57%) were female, and the mean age was 76.4 years. Mean EuroSCORE II was 9%, and the mean annular diameter was 46.9 mm. A full 95% of patients were in NYHA functional class III/IV, 28% had ascites, and 85% had peripheral edema. Most patients (75%) had a central regurgitant jet. One-third of the overall cohort had previously undergone a left-heart valve intervention, of whom a quarter had been treated with a transcatheter device.
In TriValve, the procedures involved:
- MitraClip (Abbott) in 66%
- Caval valve implantation in 9%
- FORMA (Edwards Lifesciences) in 8%
- Trialign (Mitralign) in 6%
- Cardioband (Edwards Lifesciences) in 4%
- TriCinch (4TECH) in 4%
- Other devices in 3%
These were performed as standalone procedures in two-thirds of cases. Procedural success, defined as successful device implantation and residual TR of ≤ 2+, was achieved in 72.8% of patients.On multivariate analysis, the only independent predictor of procedural failure was coaptation depth (OR 24.1; 95% CI 3.0-231.0).
At a median follow-up of 6.2 months, various measures of clinical improvement were significant: 54% of patients were in NYHA functional class I or II (P = 0.04 versus baseline), just 14% had ascites (P = 0.006), and rates of peripheral edema were more than halved at 39% (P = 0.001).
At 1.5 years, the actuarial survival rate was 82.8 ± 4%. Independent predictors of mortality at follow-up were procedural success (HR 0.18; 95% CI 0.02-2.3) and systolic pulmonary artery pressure (HR 17.0; 95% CI 1.2-252.0).
Why Tricuspid Is Unique
Speaking with TCTMD, Taramasso stressed that patients undergoing tricuspid interventions are particularly complex because the TR is secondary to heart failure and not the valve per se. As such, from an anatomical standpoint, tricuspid valve disease is more complicated than what’s seen in the aortic or even mitral arenas. There are a variety of approaches to treatment, yet “we still don’t know which device is best for each patient,” he said. Those with mainly annular dilatation would probably be best suited to an annular-based device, Taramasso suggested, while those with mainly ventricular dilatation are likely best served by a leaflet-based device like MitraClip.
Currently, the Cardioband Tricuspid Valve Reconstruction System is the only tricuspid-dedicated transcatheter device with CE Mark approval in Europe; none have regulatory approval in the United States, he said.
In an accompanying editorial, Lars Sondergaard, MD, DMSc, and Finn Gustafsson, MD, DMSc (both of Rigshospitalet, Copenhagen, Denmark), express optimism that the field will continue to move forward.
“These encouraging data bring hope to a patient population that is unserved by the current medical and invasive treatment modalities. As transcatheter tricuspid valve interventions mature and with better understanding of the best timing to intervene, controlled trials may help integrate these technologies in treatment of the failing right ventricle,” they conclude.
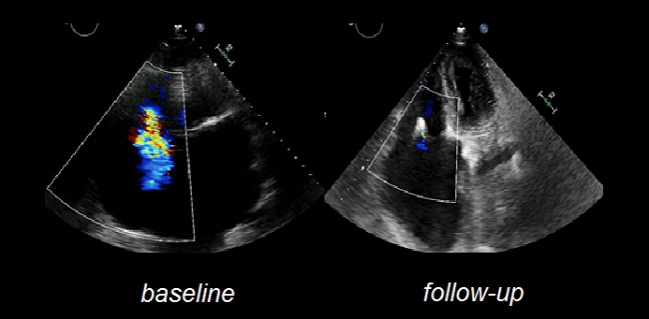
Photo Credit: adapted from Hausleiter J, et al. TRIVALVE: Evaluation of edge-to-edge valve repair for symptomatic tricuspid regurgitation. Presented at: TCT 2018. September 23, 2018. San Diego, CA.
Caitlin E. Cox is Executive Editor of TCTMD and Associate Director, Editorial Content at the Cardiovascular Research Foundation. She produces the…
Read Full BioSources
Taramasso M, Alessandrini H, Latib A, et al. Outcomes after current transcatheter tricuspid valve intervention: mid-term results from the international TriValve registry. J Am Coll Cardiol Intv. 2018;Epub ahead of print.
Sondergaard L, Gustafsson F. The potential role of transcatheter heart valve interventions in heart failure treatment. J Am Coll Cardiol Intv. 2018;Epub ahead of print.
Disclosures
- Taramasso reports serving as a consultant to Abbott Vascular, Boston Scientific, 4TECH, and CoreMedic as well as receiving speaker honoraria from Edwards Lifesciences.
- Sondergaard and Gustafsson report no relevant conflicts of interest.


Comments