TRILUMINATE Pivotal: TEER With the TriClip Benefits Patients With Severe TR
The results affirm reductions in TR severity and gains in quality of life compared with medical therapy.

NEW ORLEANS, LA—Transcatheter edge-to-edge repair (TEER) using the TriClip system (Abbott) is safe and effective in patients with symptomatic severe tricuspid regurgitation (TR), the randomized TRILUMINATE Pivotal trial shows.
After 1 year, a primary composite outcome consisting of all-cause death or tricuspid valve surgery; hospitalization for heart failure; and improvement in quality of life (QoL) according to the Kansas City Cardiomyopathy Questionnaire (KCCQ) favored TEER over medical therapy alone (win ratio 1.48; 95% CI 1.06-2.13), a finding driven by the QoL improvements.
The intervention reduced the severity of regurgitation—without fully abolishing it—and was also very safe, with a low rate of major adverse events around the time of the procedure, Paul Sorajja, MD (Allina Health Minneapolis Heart Institute at Abbott Northwestern Hospital, MN), reported here at the American College of Cardiology/World Congress of Cardiology (ACC/WCC) 2023 meeting.
The results, published simultaneously online in the New England Journal of Medicine, affirm preliminary findings from the roll-in cohort presented last year at TCT 2022, which showed few major adverse events through 30 days and a drop of at least two grades in TR severity for most patients. They’re also consistent with those of the real-world bRIGHT postapproval study conducted in Europe, where the first-generation TriClip device was approved in 2020 based on the earlier single-arm TRILUMINATE study and the next-generation G4 device was cleared in 2021. The system has not yet been approved by the US Food and Drug Administration.
“We feel these results are very meaningful for a highly symptomatic population whose quality of life is impacted by TR,” Sorajja said. “And with the excellent benefit-to-risk profile of the system, we feel that a historically untreated population will now have a treatment option to improve their quality of life.”
For Patrick O’Gara, MD (Brigham and Women’s Hospital, Boston, MA), a past president of the ACC, the findings represent “a step in the right direction.” He told TCTMD tricuspid TEER appears to be a safe procedure that leads to an improvement in quality of life, which is important to patients. “Many would complain that it’s not really a hard outcome, but I think in the current era where we’re trying to focus on patient-centered outcomes, it’s quite reasonable,” he said.
It’s a step in the right direction making heart failure patients feel better. Patrick O’Gara
Asked whether he would have expected to see differences in other outcomes, like valve surgery, between the TEER and control groups, O’Gara noted that the trial was not powered for the individual components of the primary endpoint. “That kind of gets into what’s the best way to design a trial so that we can bring it feasibly to conclusion within a reasonable period of time,” he said, acknowledging, however, that “that’s the obvious gap here.”
This is still early days for tricuspid TEER, he said, noting that the benefits of other transcatheter therapies, like TAVI and mitral TEER, became more apparent over time as devices improved and experience increased. Still, TRILUMINATE Pivotal demonstrates progress, he indicated.
“It’s not as if you’ve got a therapy here that looks like sacubitril-valsartan or an SGLT2 inhibitor, in which there’s a significant reduction in hard endpoints, for example, but it’s a step in the right direction making heart failure patients feel better,” said O’Gara.
TRILUMINATE Pivotal
For TR, which impacts both longevity and quality of life, the cornerstone of treatment has been diuretics, with surgery reserved for selected patients, Sorajja said. Transcatheter therapies have emerged for the treatment of TR, although they have not—up until this point—been studied in a randomized fashion.
TRILUMINATE Pivotal helps to fill that gap. It was conducted at 65 centers in the US, Canada, and Europe and included 350 patients (mean age 78 years; 55% women) who had symptomatic severe TR and were deemed to have at least an intermediate risk for mortality with tricuspid valve surgery. Patients were on stable guideline-directed medical therapy and/or device therapy for heart failure. They were randomized to TEER—roughly half with the first-generation TriClip system and half with the newer TriClip G4—or medical therapy alone.
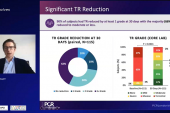
The primary hierarchical composite endpoint favored TEER at 1 year. There were no differences between the TEER and control groups in freedom from all-cause death/tricuspid valve surgery (90.6% vs 89.4%; P = 0.75) or freedom from hospitalization for heart failure (85.1% vs 87.9%; P = 0.41), with the benefit of the procedure attributed to a boost in quality of life. The KCCQ score increased by a mean of 12.3 points in the TEER arm and 0.6 points in the control arm (P < 0.001). Half of patients treated with TEER had an increase of at least 15 points, compared with 26% of controls. The proportion of patients who had worsening KCCQ scores was 18.4% in the TEER arm and 39.9% in the control arm.
At 30 days, the proportion of patients who had TR graded moderate or less was substantially higher in the TEER group (87.0% vs 4.8%; P < 0.001). The benefit was sustained out to 1 year (88.9% vs 5.6%).
Gains in KCCQ were greater in patients with moderate or less residual TR at 1 year than in those with more-severe residual regurgitation (mean increase of 16 vs 4 points). The change in KCCQ increased along with how much TR was reduced, reaching an average increase of 18 points in patients with an improvement of at least two grades.
The 6-minute walk distance declined in both groups, and although the reduction was numerically less in the TEER group (mean -8.1 vs -25.2 m), the difference was not statistically significant (P = 0.25).
The procedure was also safe, with 98.3% of patients remaining free from major adverse events at 30 days; one patient had a cardiovascular death and two patients developed new-onset renal failure. There were no cases of urgent surgery, endocarditis, device embolization, or device thrombus.
Among other safety endpoints in the 30 days after the procedure, 7.0% of patients developed single leaflet device attachment, 4.7% had a tricuspid mean gradient ≥ 5 mm Hg, and 4.7% had a major bleed. One patient (0.6%) required a new permanent pacemaker implant.
Notes of Caution
When interpreting the results, O’Gara said, “it’s important for the community to understand that this is a study that was executed by highly expert interventionalists.” Moreover, there were improvements in device design and imaging capability over the course of the study, and patients were selected for the trial by an eligibility committee based on the likelihood that the procedure would result in moderate or less TR. “Selection obviously is key here,” he stressed.
It remains unclear, then, how tricuspid TEER will perform if rolled out to a broader group of patients with severe TR. “This is not something that can be rapidly liberated among folks who don’t have the right kind of experience and team,” he said.
In that context, the results represent an incremental advancement, O’Gara said. “It’s not necessarily a leap forward at this point, but it’s early,” he said, pointing out that the earliest trials of MitraClip (Abbott) were not “particularly impressive” in terms of the reduction in the degree of MR. But since then, “with better devices and better imaging and better case selection, that technology has sort of rocketed to help a lot of people.”
The role for tricuspid TEER will be worked out over the next 5 years, O’Gara said. “The issue with TR, of course, is that we’re so limited with medical therapy, and a lot of folks would argue [that in a] heart failure population, anything that’s safe and makes people feel better is a good thing.”
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Sorajja P, Whisenant B, Hamid N, et al. Transcatheter repair for patients with tricuspid regurgitation. N Engl J Med. 2023;Epub ahead of print.
Disclosures
- TRILUMINATE was funded by Abbott.
- Sorajja consulting or serving on the advisory board for 4C Medical, Abbott Structural, Anteris, Boston Scientific, Edwards Lifesciences, Foldax, Medtronic, Philips, Siemens, Shifamed, VDyne, WL Gore, and xDot; receiving institutional research support from Abbott Structural, Boston Scientific, Edwards Lifesciences, and Medtronic; and serving as the national principal investigator for EXPAND II, Highlife (US), SUMMIT-MAC, SOAR-EFS, TRILUMINATE Pivotal, and VISTA.




Comments