For Failed MitraClip, Next Procedure Might Depend on MR Etiology
A retrospective series offers hints on operator choices and patient outcomes, plus reassurances on repeat clip procedures.
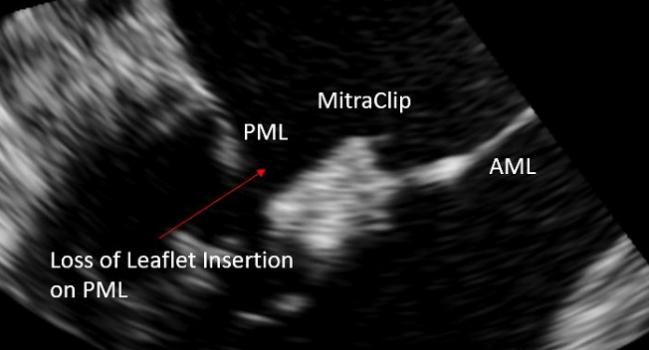
Long-axis view on TEE. PML = posterior mitral leaflet, AML = anterior mitral leaflet (Photo Credit: Hannes Alessandrini)
As MitraClip procedures continue to expand as an option for nonsurgical patients with functional or degenerative mitral regurgitation (MR), a new question will increasingly arise: what’s the best approach for treating patients whose clip procedures fail?
Now, a small, retrospective, single-center study is trying to shed some light. As Hannes Alessandrini, MD (Asklepios Klinik St. Georg, Hamburg, Germany), and colleagues write in EuroIntervention this month, the best approach may depend on the source of mitral valve dysfunction in the first place.
“There are two conclusions that we have reached,” Alessandrini told TCTMD. “The first is that we have less concern about considering a surgical intervention after transcatheter mitral valve repair in patients with primary mitral regurgitation. . . . And the second is that we also have less concern about performing a second intervention with the edge-to-edge therapy in patients where we have seen that first unsuccessful intervention.”
From a series of 824 consecutive patients who underwent MitraClip (Abbott) edge-to-edge repair at their hospital, Alessandrini and colleagues zeroed in on 96 patients with clip failure, defined as symptomatic MR > 2. Sixty-three were deemed eligible for reintervention (n = 36) or open-heart surgery (n = 27). Leaflet tears, single leaflet device attachment (SLDA), restrictions or tears caused by the clip, and/or device endocarditis were the most common causes of failure among patients selected for repeat clip procedures, whereas combinations of leaflet tear and SLDA were the most common pathomechanisms, they note. Time to repair was significantly shorter among patients ultimately treated with surgery.
But as Alessandrini stressed to TCTMD, the choice of therapy followed a clear pattern: repeat percutaneous procedures were chosen for patients with functional (secondary) MR, whereas surgery was more common among patients with degenerative (primary) MR. And while 30-day mortality was comparable in both the clip and surgery groups (16.7% and 18.5%, respectively), mortality rates over time favored the surgical group and the degenerative MR patients. As Thomas Modine, MD, PhD, and Walid Ben-Ali MD, PhD (both from Cardiologique de Haut Lévèque, Bordeaux, France), point out in an accompanying editorial, however, low patient numbers make it difficult to draw conclusions over the longer term.
What’s not known, the editorialists continued, is what transcatheter mitral valve (MV) replacement—still in its infancy—will offer MR patients deemed too sick for surgery, should investigational devices pan out in ongoing studies. In preliminary studies, they note, “transcatheter MV replacement has the advantage over transcatheter MV repair in that it is suitable for a wide range of mitral valve anatomies, including patients considered anatomically unsuitable for [repair] achieving durable MR elimination.”
If larger studies bear out, that leaves physicians with a choice to make at the time of the initial intervention, Alessandrini pointed out, since use of a MitraClip would preclude subsequent transcatheter MV replacement. “I think the MitraClip is an important therapy,” he clarified, “but maybe for patients with primary mitral regurgitation, the possibility to perform a percutaneous valve replacement is very [attractive],” whereas for patients with secondary MR, particularly those with large annuli, “valve repair using edge-to-edge may be the only way.”
Despite its limitations as an observational study, said Alessandrini, this patient series is at least reassuring that prior clip placement doesn’t rule out a second attempt, particularly in the context of functional MR.
Overcoming Challenges
A major source of data to date on failed MitraClip procedures comes from the CUTTING-EDGE registry, previously reported by Gilbert Tang, MD (Mount Sinai Health System, New York, NY). Commenting on the current study for TCTMD, Tang raised a similar point to one made by Modine and Ben-Ali, namely that reinterventions in these patients have major challenges regardless which approach is chosen.
“As shown in the CUTTING-EDGE registry,” said Tang, “MV surgery after TEER [transcatheter edge-to-edge repair] is not trivial in terms of risks, and patients who are surgical candidates with primary MR should be referred to a mitral reference center for surgical MV repair rather than TEER.”
There’s also tricuspid valve (TV) disease to consider, he added. “Those with MV [and] TV disease should have a heart team discussion on optimal management of multivalve disease rather than just do TEER for MR and then leave TR behind or try to fix it later, given that severe TR still confers poor survival in patients who have had mitral TEER.”
Tang also cautioned that it is simplistic to suggest that underlying MV pathology would be the sole determinant of the subsequent procedures—number of initial clips used, operator proficiency, other patient characteristics, and heart team consensus are all factors that might tilt a decision one way or the other, he said. Lastly, this particular series did not track outcomes in patients with failed MR in whom neither a repeat TEER or surgery was attempted.
“This does bring up an important point, which is: what do you do with these patients? Should they go to surgery, should they go to TEER, or can they be left alone with just medical therapy? And I don’t think we have the answer to that, but it needs to take into account the operator and the heart team experience as well as patient preference,” Tang advised.
Some patients, he noted, might do “perfectly fine” following a clip detachment whereas other may see regurgitation deteriorate
Shelley Wood was the Editor-in-Chief of TCTMD and the Editorial Director at the Cardiovascular Research Foundation (CRF) from October 2015…
Read Full BioSources
Alessandrini H, Dreher A, Harr C, et al. Clinical impact of intervention strategies after failed transcatheter mitral valve repair. EuroIntervention. 2021;Epub ahead of print.
Modine T, Ben-Ali W. How to eliminate mitral regurgitation definitively: the eternal dilemma? EuroIntervention. 2021;Epub ahead of print.
Disclosures
- The study authors report no conflicts of interest.
- Modine reports serving as a consultant for Boston Scientific, Medtronic, Edwards, MicroPort, GE, and Abbott, and has received research support grant from Edwards.
- Ben-Ali reports no conflicts of interest.
- Tang reports being a consultant for Abbott, Medtronic, and WL Gore





ulf landmesser