First-line Catheter Ablation Works for Post-MI VT Suppression: VANISH2
(UPDATED) Clinicians typically first turn to antiarrhythmic drugs, but switching up the order may offer patients better outcomes.
CHICAGO, IL—For patients with ischemic cardiomyopathy and ventricular tachycardia (VT) who have an implantable cardioverter-defibrillator (ICD), catheter ablation may be a better first-line therapy than antiarrhythmic drugs, according to data from the randomized VANISH2 trial.
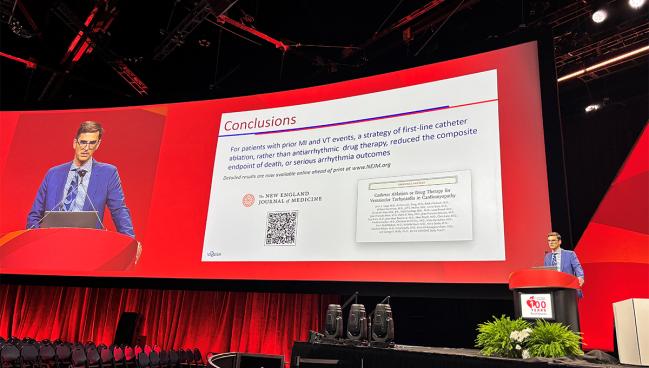
The invasive strategy offered a reduction in the composite endpoint of death or serious arrhythmia outcomes, lead author John Sapp, MD (QEII Health Science Center, Halifax, Canada), reported today at the 2024 American Heart Association (AHA) Scientific Sessions. The results were simultaneously published in the New England Journal of Medicine.
Patients with VT after MI can experience recurrent VT, and have impaired quality of life and worse survival, Sapp explained during an AHA press briefing. While ICDs are effective at treating the VT episodes, they involve painful shocks. For some patients, it’s preferable to instead suppress the VT through catheter ablation or antiarrhythmic drugs.
In the VANISH trial, “we’ve previously shown that if the antiarrhythmic drugs aren’t working, that it is better to go to ablation rather than being more aggressive with [the] drugs,” he told the media.
This time around, with VANISH2, the goal was to see how starting out with catheter ablation might impact outcomes over a drug-first approach. Both of the VANISH studies exclusively enrolled patients who already had an ICD in place but might benefit from VT suppression.
Sana Al-Khatib, MD (Duke University Medical Center, Durham, NC), who moderated the press conference, said she was quite excited to see the VANISH2 results. “I say this because for a long time, we have struggled with identifying the best treatment strategy for our patients . . . who present with ICD shocks,” she commented.
Al-Khatib continued: “The tradition has been to treat those patients with medications and really to introduce catheter ablation late in the game. And I've always questioned that. Why can't we intervene earlier so that we can actually really have an impact on things before the disease progresses? I think VANISH2 really provides us with interesting data to support that practice.”
Other trials—PAUSE-SCD, PREVENTIVE-VT, SMASH-VT, and VTACH—have supported an advantage to early ablation in VT even before ICD implantation.
VANISH2
Sapp and colleagues analyzed data for 416 patients (median age 68 years; 94% men) with a previous MI, an ICD, and clinically significant VT (defined as VT storm, receipt of appropriate ICD shock or antitachycardia pacing, or sustained VT terminated by emergency treatment) enrolled across 22 centers in three countries. Participants were randomized to either undergo catheter ablation within 14 days or receive antiarrhythmic drug therapy consisting of sotalol or amiodarone. Median follow-up was 4.3 years.
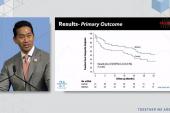
On Kaplan-Meier analysis, the primary endpoint—a composite of all-cause death during follow-up or VT tachycardia storm, appropriate ICD shock, or sustained ventricular tachycardia treated by medical intervention from 14 days after randomization—was less common in the ablation arm compared with the drug arm through 6 years (50.7% vs 60.6%; HR 0.75; 95% CI 0.58-0.97). The difference was driven by a reduction in treated sustained VT below the detection limit of the ICD after 14 days (4.4% vs 16.4%; HR 0.26; 95% CI 0.13-0.55), with the other components of the primary endpoint also supporting ablation but not reaching statistical significance.
The tradition has been to treat those patients with medications and really to introduce catheter ablation late in the game. And I've always questioned that. Sana Al-Khatib
Results were consistent across most subgroups. However, analyzing the data according to patient eligibility for the two antiarrhythmic drugs revealed an advantage for ablation only in those who could take sotalol (HR 0.64; 95%CI 0.46-0.93), not those who could take amiodarone (HR 0.86; 95%CI 0.58-1.27).
Sapp highlighted to TCTMD that VANISH2 involved two drugs in the medical-therapy arm in order to capture real-world practice patterns, with investigators stratifying randomization according to eligibility for these drugs at baseline. “Sotalol is known to be less effective but has a much better side effect profile. We don’t use sotalol in the sickest heart failure patients with the worst [VT], because the risk is high and the benefit is not enough,” he explained. Instead, for these sickest patients, the drug of choice is amiodarone.
In terms of secondary outcomes, there also was a nonsignificant trend toward fewer episodes of appropriate ICD shock or antitachycardia pacing in the catheter-ablation group as compared to the antiarrhythmic drug group (1.91 vs 6.14 events per person-year; mean difference -4.22; 95% CI -9.01 to 0.56).
For patients assigned to catheter ablation, adverse events within 30 days after treatment included two deaths (1.0%) and nonfatal events in 23 individuals (11.3%). The latter included nonfatal stroke in two patients, cardiac perforation in one, and vascular injury in five (with two of those patients having major bleeding).
For patients assigned to antiarrhythmic drugs, adverse events attributed to the therapy included one death due to pulmonary toxic effects (0.5%) as well as nonfatal events in 46 individuals (21.6%). Seven patients had drug-related pulmonary infiltrates or fibrosis, and 25 experienced GI, neurologic, thyroid-related or liver-related adverse effects that led to drug dose adjustment or discontinuation.
Notably, the VANISH2 population enrolled very few women. Sapp told TCTMD that isn’t for lack of trying.
“I don’t fully understand the low number of women in the trial,” he said, though the proportion is on par with most trials of ablation in MI. It may be due to age, given that “women on average have their heart attacks about 10 years later than men, due to protective hormonal effects and so on,” Sapp observed. Then, after the MI, it can take more than a decade for the VT to develop, so the condition may be less prevalent in women than it is in men of the same age, he added.
There’s no plausible mechanism for why “ablation versus drugs would have different outcomes in women versus men,” he noted, “There may be an effect of body size on risk of the procedure, but we don’t know that.”
Discussant Usha Tedrow, MD (Brigham and Women’s Hospital, Boston, MA), commenting on Sapp’s presentation in the late-breaking session, agreed there’s a need to carefully consider the best approach to managing these VT after MI.
Electrophysiologists “know that we give them the defibrillator to save the patient’s life [then] spend the rest of the patient’s life trying to save them from their defibrillator. ICD shocks are painful and are associated with worsened heart failure and increased mortality in patients with impaired ventricular function,” she said. While antiarrhythmic drugs are an option, they also carry toxicities.
This, said Tedrow, is where catheter ablation comes in.
Given that both arms of VANISH2 had ICDs, it would be hard to detect any survival benefit with ablation in this study, she pointed out. Even so, the trial “adds to our understanding of outcomes in this population.”
Caitlin E. Cox is Executive Editor of TCTMD and Associate Director, Editorial Content at the Cardiovascular Research Foundation. She produces the…
Read Full BioSources
Sapp JL, Tang ASL, Parkash R, et al. Catheter ablation or antiarrhythmic drugs for ventricular tachycardia. N Engl J Med. 2024;Epub ahead of print.
Disclosures
- Sapp reports research funding from Biosense Webster and Abbott as well as consulting fees/honoraria from Medtronic, Biosense Webster, Abbott, and Varian Medical Systems.




Comments