Higher Mortality After MV Surgery in Poorer Communities: STS Database
Patients with degenerative MR living in poorer neighborhoods also were less likely to be treated with MV repair.

Patients with mitral valve (MV) disease who live in economically disadvantaged communities are at a higher risk of death after surgery than those who live in richer neighborhoods, according to a new study presented this week.
Additionally, patients with degenerative MV disease living in poorer areas faced greater barriers to care: based on the area deprivation index (ADI), a neighborhood-based metric that accounts for average employment, income, housing, and education, among other factors, the rate of MV repair was 65.3% for those living in areas with the highest levels of deprivation versus 82.8% for those in areas with the lowest scores, reflecting high socioeconomic status (SES).
“Even when you select out a cohort who ought to have more repairable valves, a very tight association between socioeconomic status and rate of repair was noted,” said lead researcher Amit Iyengar, MD (University of Pennsylvania, Philadelphia, PA).
T. Sloane Guy, MD (Thomas Jefferson University, Philadelphia), who commented on the results during a press briefing, said that while the association between SES and surgical outcomes isn’t new, these findings highlight critical differences in patient care. “The conclusion that neighborhood socioeconomic data predicts the way the surgery is done, who does it, and the outcomes of the operation are well supported by the data,” said Guy. “This study clearly shows that lower socioeconomic status patients had bigger incisions, fewer repairs, and worse outcomes in terms of complications and mortality.”
Higher Mortality, Less MV Repair
Much of the prior research focused on SES and surgical outcomes involves patients undergoing CABG surgery and aortic-valve replacement, but with the introduction of complimentary therapies for the treatment of MV disease, there is a need for similar focus on SES and access to care, said Iyengar. Surgical MV repair over replacement remains recommended for patients with degenerative MV disease, with minimally invasive or robotic surgery an option for select candidates
The new results, which were presented virtually this week at the Society of Thoracic Surgeons annual meeting, are based on 137,100 adults who underwent isolated MV repair or replacement for MV disease between 2012 and 2018. Of those, 62,781 patients had primary degenerative MV disease. To look at the association between SES and outcomes, the researchers used data from the STS Adult Cardiac Surgery Database and linked these numbers to the ADI, which is a geographically derived measure that allowed them to focus on single city blocks or rural equivalents.
The patients from areas with lower SES were more likely to be female, Black, and uninsured, and to have more comorbidities, such as cerebrovascular disease and a need for preoperative dialysis. Those from more-deprived neighborhoods were less likely to have degenerative mitral valve pathology and a lower rate of elective procedures. Patients with high SES, on the other hand, traveled further for surgery and were treated by higher-volume surgeons.
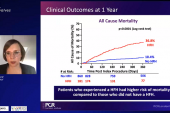
Stratified into quintiles based on ADI (a lower ADI representing higher SES), those in the poorer neighborhoods were less likely to undergo MV repair and had a higher rate of death at discharge. Overall, 71.9% of patients with the highest SES (lowest ADI quintile) underwent MV repair compared with just 50.5% with the lowest SES (highest ADI quintile). With respect to mortality at discharge, the rate was 1.9% among patients with the highest SES compared with 3.8% for patients with the lowest SES. This higher rate of death at discharge was not proportionate to the 30-day STS predicted risk score.
In their model, patients living in the most economically disadvantaged neighborhoods had a 1.5-fold higher risk of death compared with the median ADI. In contrast, there was a lower risk of death at discharge among those in less-deprived areas.
Guy said there have been numerous papers showing sex, race, and SES are factors influencing clinical outcomes, leading to conclusions that some patients are getting worse treatment.
“Of course, the issue is more complicated,” said Guy. Access to care, including the ability to travel to high-volume MV repair specialists “is clearly a discriminator that negatively impacts those living in socioeconomic deprived neighborhoods,” he said. Such patients appear to have limited resources and options, as well as information about available therapies, compared with those living in rich neighborhoods.
Guy noted that a 2017 study showed that individual surgeon volume was associated with MV repair rates, as well as freedom from reoperation and survival. The new findings showing differences in outcomes across SES suggests “that much of the difference could be explained simply by the lower socioeconomic status patients being denied access to such high-volume surgeons for a variety of reasons.”
Iyengar pointed out, however, that even after adjusting for differences in patient comorbidities, demographics, and racial disparities across the different neighborhoods, “we still saw an independent association between the area deprivation index and outcomes, suggesting that neighborhood-level disparity influences outcomes in ways beyond pure demographic and hospital- or surgeon-level factors.”
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Iyengar I. Neighborhood socioeconomic status independently predicts outcomes after mitral valve surgery: an STS national database study. Presented at: STS 2022. January 31, 2022.
Disclosures
- Iyengar reports no conflicts of interest.



Comments