Intravascular Imaging During PCI Should Be a Performance Metric, Researchers Say
Not everyone agrees: one expert says it would be more helpful to consider imaging as a quality measure at the local level.
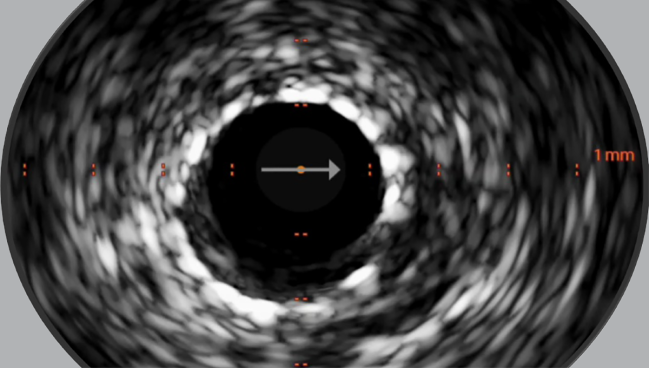
Photo Credit: Adapted from Shlofmitz E. IVUS & OCT image interpretation made easy. Presented at: Cardiovascular Interventions 2024. Torrey Pines, CA.
Use of intravascular imaging during PCI, which has been increasing within the Veterans Affairs (VA) system, should be considered as a formal performance measure, researchers propose.
IVUS or OCT, when reliably assessed at both the hospital and physician levels, enable the identification of high-quality centers and operators, lead author Elliot Stein, MD (University of Washington Medical Center, Seattle), and colleagues report in a study published online recently in Circulation: Cardiovascular Interventions.
The substantial variation in the deployment of imaging was driven mostly by hospital and physician—but not patient—factors, ranging from no use of intravascular imaging to use in all cases, they report.
Prior studies, including multiple randomized trials involving various subsets of patients, have shown the benefit of using intravascular imaging routinely during PCI, but adoption in the United States remains low. In earlier reports, just 8% to 16.5% of all PCIs incorporated such imaging.
The accumulated evidence suggests, however, “that intravascular imaging use should be more ubiquitous,” Stein told TCTMD. He and his colleagues believe that intravascular imaging is ready to be introduced as a formal performance measure that can encourage greater adoption.
“With our study’s findings, we now know that we can measure intravascular imaging use during PCI in a high-throughput fashion in the large VA healthcare system, and that assessing intravascular imaging use is a reliable measure of performance of physicians and hospitals,” Stein said. “If we agree that intravascular imaging use is beneficial for patients, and we know that we can measure it in a reliable way, then it’s incorporation into the guidelines should be considered.”
Its use as a performance measure “could be done on a more local basis initially—like at a hospital or a healthcare system—and then perhaps will become more widespread nationally,” he added.
But Dmitriy Feldman, MD (Weill Cornell Medicine, New York, NY), who wrote an accompanying editorial with Adam Vohra, MD (University of Chicago, IL), told TCTMD that use of IVUS or OCT during PCI is not quite ready to be implemented as a formal performance measure.
“We don’t think it’s appropriate for public reporting or [as a] pay-for-performance metric,” he said. “I don’t think making it a formal performance measure at this point would be helpful because I think it may incentivize wrong behavior, meaning that imaging in 100% of cases without an ability to thoughtfully interpret the imaging that you do and use the data to optimize the PCI result . . . is not going to lead to a meaningful improvement in outcomes. Imaging itself doesn’t do that. It’s using the imaging, using the data, and then optimizing your PCI based on that data [that is] going to lead to improved technical results and then a long-term clinical improvement.”
He added, however, “locally, institutionally, it could be a very useful quality metric.”
The VA CART Program
Although there have been “growing calls” for the routine use of intravascular imaging, there has never been a formal assessment of its performance as a measure of quality, the investigators say. To explore that question and other issues, they turned to the VA Clinical Assessment Reporting and Tracking (CART) program, which contains information on all PCIs performed at VA hospitals.
Use of IVUS and OCT during PCI increased from 12.3% in 2010 to 43.1% in 2022, with acceleration of the trend starting in 2018. Variability was high, with median usage of 33.5% of all PCIs at the hospital level and 32.4% at the physician level in 2022.
Patient factors tied to use included chronic kidney disease, heart failure, and nonemergent presentation, and lesion factors included chronic total occlusion, calcification, bifurcations, left main disease, and LAD disease. In addition, high-volume cath labs and hospitals with cardiothoracic surgery backup were more likely to deploy IVUS or OCT.
Though imaging was more frequent among patients with complex coronary disease, most of the variability was attributed to factors at the hospital and physician levels (54% and 33% of the variability, respectively). Only 1.1% was related to patient and coronary lesion characteristics.
Regarding use of intravascular imaging as a pass/fail performance measure, Stein et al found that reliability was high, with a Pearson correlation coefficient of 0.99 at the hospital level and 0.96 at the physician level.
This “meets National Quality Forum standards for validity and reliability of a performance measure and should be implemented by local, regional, and national organizations to promote PCI quality and improved patient outcomes in the United States,” they write.
In this study, however, use of IVUS or OCT was not associated with significant differences in the risks of several clinical outcomes at 1 year, including MACE, mortality, rehospitalization for MI, repeat revascularization, and stroke. Stein stressed, too, that these observational data should not invalidate the findings of multiple randomized trials demonstrating meaningful impacts on clinical outcomes.
Working to Increase Intravascular Imaging During PCI
The study provides a mixed view of the intravascular imaging landscape, according to Alexander Truesdell, MD (Inova Heart and Vascular Institute, Falls Church, VA), who led a state-of-the art review on the subject from American College of Cardiology’s Interventional Council.
It’s good to see that uptake of IVUS and OCT increased over the study period and that tracking the metric may help increase uptake even further, he commented to TCTMD.
On the other hand, indications that much of the variability in imaging use lies at the hospital and physician levels “is a little bit unfortunate, because really in the perfect, ideal world, all of our clinical decisions on whether to use intracoronary imaging or not should be based on the patient—the patient’s anatomy, the patient’s clinical presentation—and not on what hospital, what cath lab, the patient presents to or what doctor performs the procedure,” said Truesdell.
Major contributing factors for the underuse of intravascular imaging during PCI likely include a discomfort with image interpretation and a perception that it increases procedural time, Truesdell said, adding that, in fact, many cath labs see their workflows speed up with imaging due to increased efficiency.
There may also be a perceived lack of clinical benefit when it comes to using intravascular imaging in all-comers, he said, because the randomized trials were conducted in specific patient subsets, such as those with left main disease, bifurcations, or long lesions.
“To me, that does not preclude use in all-comers,” Truesdell said, advocating for wider use so that operators remain adept at performing such imaging. “If there’s not an intentional practice and rehearsal, and you’re not getting used to image interpretation and how to troubleshoot and hook up the device and you’re not advocating for use in your lab, I think you’re really never going to get over a certain threshold,” he said. He likened it to what happened with transradial access for PCI, where uptake lagged behind the evidence by several years and practice changed “through a lot of carrot and stick initiatives.”
In that context, Truesdell endorsed implementing intravascular imaging use during PCI as a formal performance measure. “That doesn’t necessarily mean there have to be penalties associated with it. . . The best way to do that is through incentive programs and sort of carrot-type stuff initially, but one could see as the evidence continues to accrue that that could transition to stick initiatives.”
Ultimately, he said, “I just hope [intravascular imaging during PCI] gets up to a class I, level of evidence A recommendation in the next US guidelines, as it is in the European guidelines.”
For Feldman, greater use of intravascular imaging in the US will hinge on additional trial data, particularly in all-comers; improved competency among operators in performing, interpreting, and using imaging results to optimize procedural results; continued improvements in imaging quality and systems; and fewer reimbursement and regulatory challenges.
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Stein EJ, Mesenbring E, Smith T, et al. Intravascular imaging as a performance measure for percutaneous coronary intervention. Circ Cardiovasc Interv. 2025;18:e014528.
Vohra AS, Feldman DN. Putting the cart before the horse: intravascular imaging as a performance measure. Circ Cardiovasc Interv. 2025;18:e015004.
Disclosures
- The study was supported by the VA Clinical Assessment, Reporting, and Tracking Program.
- Feldman, Vohra, and Stein report no relevant conflicts of interest.





Comments