OCCUPI: OCT Guidance Improves Outcomes in Complex PCI
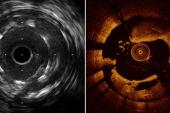
Notable in the trial was the use of OCT for stent optimization, which investigators say should be a key takeaway.

LONDON, England—Patients with complex CAD undergoing PCI have a lower incidence of cardiac death, MI, stent thrombosis, or ischemia-driven target vessel revascularization 12 months later if their procedures are done with adjunctive OCT as opposed to angiography, results from the OCCUPI trial show.
“These findings support the therapeutic benefit of OCT as an effective intravascular imaging modality in treating complex lesions,” Byeong-Keuk Kim, MD, PhD (Severance Hospital, Yonsei University College of Medicine, Seoul, South Korea), reported earlier this week at the European Society of Cardiology (ESC) Congress 2024.
While numerous studies have supported the benefits of intravascular imaging in complex PCI procedures, most of these studies were done exclusively or primarily with IVUS, Kim said.
Other trials, including last year’s ILUMIEN IV and OCTOBER, have studied different patient groups or lesions, delivering mixed results. OCCUPI extends the evidence base by focusing on patients with both complex lesions and challenging clinical scenarios.
OCT Before and After
OCCUPI investigators enrolled 1,604 patients between January 2019 and September 2022 at 20 centers in South Korea, randomizing them equally to angiography-guided DES implantation or an OCT-guided procedure. Complex coronary lesions included chronic total occlusions, longer lesions, bifurcations, calcified vessels, unprotected left main, and small vessels as well as, notably, acute MI (both STEMI and NSTEMI).
At the time of PCI, final stent diameter and postprocedure minimal lumen diameter were each significantly bigger in the OCT group (3.2 vs 3.0 mm and 2.75 vs 2.59 mm, respectively); then, postprocedure diameter stenosis was significantly reduced in patients treated with OCT guidance (12% vs 14%; P < 0.001 for all).
At 1 year, the rate of the composite endpoint of cardiac death, MI, stent thrombosis, or TVR was significantly lower in the OCT-guided patients: 4.6% versus 7.4% (HR 0.62; 95% CI 0.41-0.93). Cardiac deaths were numerically lower in the OCT group (one versus five), and rates of spontaneous MI were significantly reduced (0.9% vs 2.4%; HR 0.36; 95% CI 0.15-0.86).
In OCCUPI, operators were encouraged to also use OCT to optimize stent implantation, and fully 545 patients underwent OCT following the initial stent placement. In a comparison of patients who did and didn’t undergo stent optimization with OCT, the cumulative incidence of the primary endpoint was significantly lower at 2.9% versus 8.6%, respectively, a statistically significant difference (HR 0.33; 95% CI 0.17-0.65).
“In this multicenter randomized OCCUPI trial involving patients with PCI with DES implantation because of anatomically complex lesions, OCT-guided PCI led to a reduced risk of 1-year composite of cardiac death, MI, stent thrombosis, or TVR compared with angiographically guided PCI,” Kim summarized.
This was driven by reductions in spontaneous MI and TVR without a corresponding increase in contrast-induced nephropathy, he added. “In the OCT-guided PCI group, patients who met the prespecified OCCUPI-OCT optimization criteria—acceptable expansion, apposition, and edge dissection—had a significantly lower MACE rate compared to those with suboptimization.”
Guideline Supported
Discussing the findings after their Hot Line presentation Monday, Ulf Landmesser, MD (Deutsches Herzzentrum Charité, Berlin, Germany), pointed out, like Kim, that the bulk of the evidence supporting intravascular imaging comes from the IVUS literature. “Therefore, it's very important that we have more data now from the OCCUPI study for OCT—the more recent imaging technology,” he said. “The OCCUPI study provides further important support for the conclusion that OCT imaging guidance leads to improved clinical outcomes in PCI in patients with complex coronary lesions—so not in every PCI patient, [but in those] with complex coronary lesions, which were studied in the present trial.”
The new ESC guidelines for the management of chronic coronary disease, released earlier in the meeting, gave a class Ia recommendation to either IVUS or OCT for imaging guidance in patients with complex CAD, Landmesser added. Another important result from OCCUPI, he said, is “that these patients who achieved optimized criteria aimed for in the imaging guidance had significantly better outcomes.”
Asked by session co-chair Stephan Achenbach, MD (University of Erlangen, Germany), which OCT run is the “more important one—pre or post,” Kim replied that both the planning and the optimization runs are important. To him, however, “stent optimization is more important, as was shown in this study—the post-stent evaluation is very, very important,” Kim said.
Rasha Al-Lamee, MBBS, PhD (Imperial College London, England), also chairing the session, congratulated Kim and colleagues for “leading the effort to give us more data in the intravascular imaging space.” She added: “It feels like we've been on [a] long expedition to the point at which we get this class Ia recommendation.”
Commenting on the study for TCTMD, Pablo Lamelas, MD (Fundación Favaloro, Buenos Aires, Argentina), also praised the new guidelines for embracing intravascular imaging.
Last year’s OCT trials were added to a network meta-analysis led by Gregg Stone MD (Icahn School of Medicine at Mount Sinai, New York, NY), that conclusively established a benefit of intravascular imaging, Lamelas pointed out. As such, “this OCCUPI study shows no big news,” he said. “It’s good news, but not big news. . . . This simply reinforces that in complex PCI, use of intravascular imaging, in this case through OCT, has benefit.”
The Stone meta-analysis also clarified that while OCT and IVUS may have advantages in certain scenarios, most of the time they can be used interchangeably, he added.
At this point, if operators or hospitals still aren’t using intravascular imaging in their complex PCIs, they are likely prevented from doing so by prohibitive costs, lack of access to the equipment, a resistance to “believe” the data, or a reluctance to learn how to use it, Lamelas said. “Many doctors [of the] old school, let’s say, don’t feel comfortable learning and doing this new technique.”
On the other hand, he continued, “there are places in the world where they use systematic IVUS or OCT in every PCI case. That’s probably the future, but we are not there yet because in the lower-complexity procedures the added value of doing OCT or IVUS is more debatable” from a cost-effectiveness standpoint, something centers looking to adopt intravascular imaging may want to consider.
“For simple, noncomplex, stable cases, we can have good outcomes without the need for intravascular imaging,” said Lamelas.
Shelley Wood was the Editor-in-Chief of TCTMD and the Editorial Director at the Cardiovascular Research Foundation (CRF) from October 2015…
Read Full BioSources
Kim B-K. The OCCUPI randomized clinical trial: OCT-guided PCI for the complex lesions. Presented at the European Society of Cardiology Congress 2024. September 2, 2024. London, England.
Disclosures
- Kim reports no relevant conflicts of interest.
- OCCUPI was funded by Abbott Vascular and supported by the Cardiovascular Research Center (Korea).



Comments