Outcomes Suffer When Device-Related Thrombus Persists or Recurs After LAAO
Many DRTs either don’t resolve with treatment or recur later, raising questions around optimal management approaches.
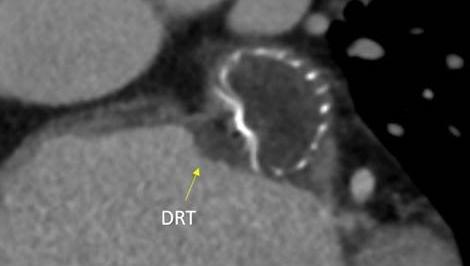
Device-related thrombus (DRT) that develops after left atrial appendage occlusion (LAAO) either persists or recurs despite initially resolving with treatment in about one-third of cases, a retrospective study shows.
This “unfavorable evolution” is associated with a greater risk of thromboembolic events compared with DRT resolution (HR 2.13; 95% CI 1.15-3.94), according to researchers led by Jules Mesnier, MD (Quebec Heart and Lung Institute, Laval University, Canada), and Trevor Simard, MD (Mayo Clinic, Rochester, MN).
DRT has been reported at a rate of 3% to 4% after LAAO, and it remains a major issue with the procedure. Most, but not all, studies have demonstrated a relationship between DRT and increased risk of ischemic events.
Study author Mohamad Alkhouli, MD (Mayo Clinic), referring to this new analysis, told TCTMD, “I don’t want to say it sounds the alarm, because the alarm has been sounded before, but it really brings DRT back to the forefront.” This issue, he continued, has been pushed aside somewhat as LAAO technology has evolved. “I don’t think it should be on the side,” he said. “I think it should be in the forefront of our long-term vision of left atrial appendage occlusion altogether and how to solve this.”
Although newer devices have features aimed at reducing DRT, it remains to be seen whether they will work. In the meantime, Alkhouli said, “Do not ignore DRT. Even if it’s [infrequent], this is a preventative procedure that is meant to prevent a small odds of stroke, so we shouldn’t ignore DRT. It’s still a very prognostically impactful phenomenon, and it is very difficult to manage.”
‘Unfavorable Evolution’ More Likely With Larger Clots
In clinical practice, it has become apparent that even though most DRTs resolved with anticoagulation, some patients had clots that persisted despite treatment or resolved initially and then came back, Alkhouli said. The current study, published in the November 27, 2023, issue of JACC: Cardiovascular Interventions, which builds on a prior analysis from this group, delves further into these difficult-to-treat cases.
The LAAO-DRT international, multicenter registry included patients diagnosed with DRT by transesophageal echocardiography (TEE) or CT after LAAO, with the current analysis focusing on the 214 patients (mean age 75.6 years; 37.4% women) who had subsequent imaging after the initial diagnosis. A mix of LAAO devices were used, but the most common were the first-generation Watchman (Boston Scientific), used in 64.5%, and the Amplatzer Amulet (Abbott), used in 15.4%.
DRT was most frequently treated with anticoagulation (56.5%), although some patients received a combination of anticoagulation and antiplatelet therapy (29.9%), single antiplatelet therapy (4.7%), dual antiplatelet therapy (4.2%), or no treatment (4.7%).
Overall, DRT resolved in 71.5% of cases, persisting in the remaining 28.5%. Factors associated with persistence were a larger initial DRT size (OR 1.08 per 1-mm increase; 95% CI 1.02-1.15) and female sex (OR 2.44; 95% CI 1.12-5.26).
Among those who had a DRT that resolved and then underwent subsequent imaging, 17.1% had a recurrent clot.
Taken together, either persistent or recurrent DRT occurred in 35.0%. The only factor independently associated with such “unfavorable evolution” was a larger initial thrombus size (OR 1.09 per 1-mm increase; 95% CI 1.03-1.16).
The rate of thromboembolic events (ischemic stroke or peripheral embolism) was higher among those with either persistent or recurrent DRT than among those with a resolved clot (26.7% vs 15.7%).
Questions About DRT Management
In an accompanying editorial, Issam Moussa, MD, MBA (University of Illinois Urbana-Champaign), points out discrepancies across this and other studies that have examined DRT after LAAO, which could be related to differences in imaging or treatment practices. But he calls the study “a very valuable addition to the literature.”
Speaking with TCTMD, he said that there remain questions about the incidence of DRT because of when post-LAAO imaging is performed in practice (typically at 6 weeks) and about optimal treatment (anticoagulation versus antiplatelet therapy). A randomized trial to answer the latter question would prove difficult given the low rate of DRT and the large number of patients that would be needed to have sufficient statistical power for a comparison, he indicated.
As for how big of a problem DRT following LAAO is, Moussa said “it is important but it’s not a major limitation of therapy.” He noted that after accounting for the DRT cases that resolve with treatment, there’s a rate of about 1% to 1.5% that don’t resolve, and some of those patients will have thromboembolic events tied to the issue. Moussa likened that to stent thrombosis after PCI, saying “it is an important adverse event with this procedure, but in terms of absolute impact on the larger population, it's small.”
I think there is a tendency now in the field to minimize the frequency and the impact of DRT. I think that is wrong, and I think we should be vigilant. Mohamad Alkhouli
For his part, Alkhouli indicated that operators need to remain vigilant when it comes to DRT, pointing to the uncertainties around the best ways to perform surveillance for the issue and to treat it.
There have been some proposals for DRT management, and Alkhouli and his colleagues outline those in a separate state-of-the-art review published in the same issue of JACC: Cardiovascular Interventions. The review also contains a classification system for DRT to help distinguish it from hypoattenuated thickening, which has been seen in 50% to 60% of patients in some studies.
The two papers together will help guide clinicians when it comes to DRT as researchers seek to answer some of the remaining questions in this area, Alkhouli said.
DRT is “the only major limitation that may affect the future of left atrial appendage closure,” Alkhouli said. “I think there is a tendency now in the field to minimize the frequency and the impact of DRT. I think that is wrong, and I think we should be vigilant and really put some effort together to study this further and try to solve it once and for all.”
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Mesnier J, Simard T, Jung RG, et al. Persistent and recurrent device-related thrombus after left atrial appendage closure: incidence, predictors, and outcomes. J Am Coll Cardiol Intv. 2023;16(22):2722-2732.
Alkhouli M, Alarouri H, Kramer A, et al. Device-related thrombus after left atrial appendage occlusion: clinical impact, predictors, classification, and management. J Am Coll Cardiol Intv. 2023;16(22):2695-2707.
Moussa I. Predicting behavior of device-related thrombus after left atrial appendage occlusion: the Heisenberg’s uncertainty principle applies. J Am Coll Cardiol Intv. 2023;16(22):2733-2735.
Disclosures
- Alkhouli reports having served as a consultant for Boston Scientific.
- Mesnier, Simard, and Moussa report no relevant conflicts of interest.





Comments