Peridevice Leaks After LAA Occlusion Signal Poorer 5-Year Outcomes
Leaks must be taken seriously, but “there’s no need for panic” because overall risk remains low, Boris Schmidt says.

Patients who have peridevice leaks detected a year after left atrial appendage (LAA) occlusion fare worse over the next several years than those whose appendages are completely sealed off, an analysis of pooled data from multiple studies of the first-generation Watchman 2.5 device indicates.
Leaks ≤ 5 mm in size were associated with a higher rate of ischemic stroke or systemic embolism through 5 years of follow-up compared with no leaks, researchers led by Srinivas Dukkipati, MD (Icahn School of Medicine at Mount Sinai, New York, NY), report.
That was mostly due to a greater risk of nondisabling stroke among patients with incompletely occluded appendages, with no difference between groups in disabling/fatal stroke. Leaks were not associated with risks of CV/unexplained death or all-cause death.
“Minimally, these data highlight the importance of optimizing device positioning during the initial implantation procedure to minimize the possibility of leak, a goal facilitated by newer LAA closure devices such as the Watchman FLX and Amulet devices, which have reduced 1-year peridevice leak rates,” the investigators write in the August 2, 2022, issue of the Journal of the American College of Cardiology. The results were previously presented at the American Heart Association 2021 Scientific Sessions.
In addition, “it seems reasonable to consider closing persistent leaks, particularly in patients with peridevice leaks suffering thromboembolic events,” they say, pointing to methods like radiofrequency ablation, coil embolization, and closure with plugs or ductal occluder devices. “However, it should be emphasized that future studies are needed to determine whether closing persistent peridevice leaks does indeed reduce subsequent thromboembolic risk.”
Dukkipati et al stress the importance of considering these findings in the context of low overall event rates, regardless of the presence of leaks. They note that the overall ischemic stroke rate was 1.6% per year among patients treated with the Watchman 2.5 device, which is about the same as what would be expected if they had received oral anticoagulation instead (1.7% per year) and lower than what would be anticipated in a cohort of patients who received no stroke prophylaxis (about 6% per year).
Growing Evidence That Leaks Are Clinically Important
Percutaneous LAA occlusion has emerged as an alternative to oral anticoagulation for stroke prevention in patients with atrial fibrillation. After the procedure, incomplete closure is relatively common, resulting in peridevice leaks. In the original trials of the first-generation Watchman 2.5 device (Boston Scientific), a postimplantation peridevice leak of 5 mm or less was considered acceptable, and a look at data from the PROTECT-AF trial suggested leaks this small were not associated with heightened risks of thromboembolic events. That analysis was limited, however, by low numbers of patients and events.
In recent years, data indicating that peridevice leaks of 5 mm or less are clinically important have emerged. One case-control study demonstrated that leaks of that size were associated with a greater risk of stroke/TIA, and a large registry study presented earlier this year at the American College of Cardiology 2022 Scientific Session showed that residual flow from the appendage was associated with a significantly higher rate of stroke, TIA, or systemic embolism.
Dukkipati et al explored the issue using pooled data from the randomized PROTECT-AF and PREVAIL trials of the Watchman 2.5 device versus warfarin and the nonrandomized CAP2 registry. The analysis included a total of 1,054 patients (mean age 74; 65% men), who had a mean CHA2DS2-VASc score of 4.1.
All had the completeness of LAA occlusion assessed using transesophageal echocardiography (TEE) at 45 days and 1 year. At 45 days, 38.3% of patients had a peridevice leak of 5 mm or less and 60.2% had no leak. Those figures were 27.7% and 71.6%, respectively, at 1 year. A small number of patients had leaks larger than 5 mm, and they were excluded from the main analyses.
Over time, most leaks (55%) present at 45 days either decreased in size or disappeared entirely.
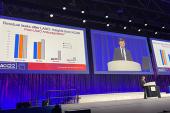
The presence of leaks of 5 mm or less at 45 days was not associated with risk of any of the clinical outcomes assessed in the study. Those that persisted at 1 year, however, were associated with a greater 5-year risk of ischemic stroke or systemic embolism (9.5% vs 5.1%; adjusted HR 1.94; 95% CI 1.15-3.29). There was a significant difference in nondisabling stroke (6.4% vs 3.2%; HR 2.03; 95% CI 1.06-3.89), but not disabling/fatal stroke (1.3% vs 1.7%; HR 0.71; 95% CI 0.20-2.53). Mortality was not associated with leaks at either time point.
As for the lack of a relationship between incomplete closure at 45 days and longer-term clinical outcomes, the investigators say it could be related to the changing antithrombotic regimen around that time (switching over from oral anticoagulation to dual antiplatelet therapy) and to the temporal changes in leaks between 45 days and 1 year.
‘No Need for Panic’
Commenting for TCTMD, Boris Schmidt, MD, who wrote an accompanying editorial with K.R. Julian Chun, MD (both Agaplesion Markus Krankenhaus, Academic Teaching Hospital of Goethe University, Frankfurt, Germany), noted that previously, implanters of LAA occlusion devices “were always pleased and happy with device leaks smaller than 5 mm, and we would have stopped oral anticoagulation in this particular patient.”
With this and other studies, however, “now of course we have to rethink that strategy,” Schmidt said, noting that recent data indicates “we are doing quite poorly in completely occluding left atrial appendages.”
Newer devices like the Watchman FLX and the Amplatzer Amulet (Abbott) have brought leak rates down, but “there’s still room for improvement,” which will likely come in the form of technological advances rather than refinements in operator technique, Schmidt said. “We cannot be happy with the data. It’s better, yes, and it sends a positive signal, but we need to continue looking at factors to improve that data because if you want to occlude the appendage, you have to occlude the appendage and it has to be 100%.”
There are no randomized data to guide clinicians in what to do when a peridevice leak persists a year after LAA occlusion, and until that evidence is available, it’s best to individualize management decisions, according to Schmidt.
“If the patient is able and willing to take oral anticoagulation, I would probably resume and keep the patient on oral anticoagulation,” he said. “If the patient has, let’s say, bleeding risk factors or is not willing to continue oral anticoagulation on top of the device . . . then I would look at interventional closure techniques.”
When it comes to monitoring patients for peridevice leaks, Schmidt said those who have residual flow at 45 or 90 days should probably come back in for a repeat TEE at 1 year, whereas those without leak on an early TEE probably don’t need a repeat assessment.
Ultimately, Schmidt said leaks need to be taken seriously given the data suggesting an impact on clinical outcomes. “However, there’s no need for panic because the overall risk still stays very, very low,” even in those with incompletely sealed appendages.
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Dukkipati SR, Holmes DR Jr, Doshi SK, et al. Impact of peridevice leak on 5-year outcomes after left atrial appendage closure. J Am Coll Cardiol. 2022;80:469-483.
Schmidt B, Chun KRJ. Peridevice leaks: the plot hole of left atrial appendage closure for stroke prophylaxis. J Am Coll Cardiol. 2022;80:484-485.
Disclosures
- The PROTECT-AF, PREVAIL, and CAP2 studies were funded by Boston Scientific.
- Dukkipati reports having received a research grant from Biosense Webster and having equity in Manual Surgical Sciences and Farapulse (acquired by Boston Scientific).
- Schmidt and Chun report having received research grants and speaker fees from Boston Scientific and Abbott.




Comments