Surgical Outcomes After Failed TEER: More Insights, Red Flags From CUTTING-EDGE
(UPDATED) Patients undergoing surgical valve replacement after failed TEER tended to fare worse, highlighting some innovation opportunities.

PHOENIX, AZ—The risks of surgical reintervention for a failed mitral valve transcatheter edge-to-edge repair (TEER) are “not negligible,” a new analysis of the CUTTING-EDGE registry confirms, with mitral valve (MV) replacement surgeries associated with more potential hazards than repairs.
“Compared to mitral valve repair, mitral valve replacement has significant risks after failed TEER due to multiple factors,” said Syed Zaid, MD (Houston Methodist Debakey Heart & Vascular Center, TX), who presented the analysis here at TVT 2023. “Early referral may be crucial.”
Speaking with TCTMD, Zaid also stressed the need for innovation in this space that’s specifically geared toward making repair a more-feasible procedure. "We need to have technological advances in terms of developing mechanisms to pry open TEER devices to improve repairability of mitral valves after failed TEER,” he said. “That should be the big focus for future technologies.”
Worldwide, more than 150,000 TEER procedures have now been performed for primary and secondary mitral regurgitation (MR), yet there are limited data on how patients fare if their TEER procedures fail, warranting surgical intervention. The international CUTTING-EDGE registry is tracking these patients: prior snapshots have emphasized the risks of surgical intervention according to the time of TEER failure, as well as the influence of underlying MR pathology on subsequent surgical risk.
We need to have technological advances in terms of developing mechanisms to pry open TEER devices to improve repairability of mitral valves after failed TEER. Syed Zaid
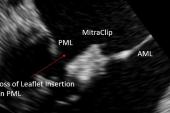
This latest analysis sought to compare outcomes following surgical repair versus replacement for a previously placed device. The original MitraClip device (Abbott) was used in more than half of the patients in the registry, followed by the NT, NTR, and NTX iterations. Just two patients were treated with the newest G4 device, and only four received the Pascal clasping device (Edwards Lifesciences).
Thirty-four centers around the world are participating in CUTTING-EDGE. The current analysis looked at outcomes in 332 patients who underwent TEER procedures as early as 2005, then needed a surgical reintervention at some point between 2009 and 2020.
The vast majority of these surgeries were MV replacement (92.5%) and the remainder repair, with outcomes compared at 30 days and 1 year.
As Zaid showed here, the underlying pathology leading to TEER in the first place was mostly primary MR, reflecting the fact that this indication was granted much earlier than secondary MR. Just 38.5% of cases were secondary MR and 14% were mixed.
Surgery to the Rescue
At the time of the surgery, the median STS PROM score for MV repair was 4.0%. Half of patients (51.3%) were deemed to be low or intermediate surgical risk by the heart team, and the reasons for surgical reintervention were recurrent MR in one-third of the patients, residual MR in an additional 28.7%, a single-leaflet device attachment in 25%, a partial leaflet detachment in 21.8%, and mitral valve stenosis in 14.5%.
Operators, helped by newer, repositionable devices, are already getting better at trimming down rates of leaflet detachment, Zaid noted. The residual MR and mitral valve stenosis rates also point to areas where interventionalists could do more to curb rates of future failure, he said. “These are things that we can optimize.”
There were no real differences in mitral regurgitation, tricuspid regurgitation, or right ventricular dysfunction prior to TEER, post-TEER, or before surgery between patients subsequently treated with surgical MV repair versus replacement. The time to surgery was also no different between groups.
Operative characteristics, however, showed that patients sent for urgent surgery were more likely to get MV replacement than repair, and tended to also need more concomitant tricuspid valve surgery. And while in-hospital outcomes were roughly similar in patients treated with replacement versus repair, longer-term outcomes followed a different pattern. By 30 days, 4% of MV repair patients had died as compared with 17.7% of replacement patients, with a statistically significant difference evidence by 1 year (10.5% vs 33.3%; P = 0.041).
Cumulative survival out to 24 months also favored MV repair over replacement, at 90.3% versus 70.4%. As previously shown, elective reinterventions were more likely to be repair procedures, whereas urgent reinterventions were more likely to be replacements.
Room to Improve
There are a number of key takeaways, said Gilbert Tang, MD, MBA (Mount Sinai Health System, New York), principal investigator for the CUTTING-EDGE registry.
“From my perspective, when you do your first-time TEER, number one is you want to make sure you have mild or better MR coming out,” he told TCTMD. As a recent STS/ACC TVT Registry analysis of primary MR patients treated with TEER released earlier this year makes clear, “the percentage of patients with 1+ or better MR is not that high,” Tang said. “It's only around 67%, which to me as a surgeon would be pretty unacceptable if you start doing TEER in lower-risk patients. So we need to, as a community, really try to optimize the outcomes initially.”
Recent results with the latest-generation MitraClip, the G4, suggest that it’s possible to get rates of 1+ or better MR at 30 days of nearly 90%, he added. The lower the rates of residual MR, the lower the rates of surgery for failed TEER down the road.
“But if they do fail, and even surgical repairs can fail, then you want to refer these patient earlier for surgical intervention,” Tang continued. Patients referred later tended to be more sick—with more right heart failure and more tricuspid valve interventions. “That makes the operation more complex than just the isolated mitral valve surgery—you now have to do other things in addition, and that increases the risk. And, if you have to urgently operate on them because they're in shock or they're in overt heart failure, that increases the surgical risk, too.”
Both Zaid and Tang had ideas for how innovation could help make repair a more-feasible option after TEER. That might include techniques for prying apart the clips and clasps after reendothelialization and healing to minimize the damage to the leaflet and maximize the amount of salvageable tissue, or development of devices themselves that have mechanisms for decoupling to create a single orifice again.
Moreover, said Zaid, other leaflet modification technologies and techniques, annular devices, or transcatheter MV replacement, in select anatomies, “may improve repairability of the mitral valve after failed TEER and perhaps obviate the need for surgery.”
“I think there's a lot of opportunities from this registry that we can learn from to actually push the field forward,” Tang added.
Importantly, he noted, the registry did not capture patients who were turned down for surgery, did not undergo surgery, or elected not to undergo a subsequent surgery, “so there’s some selection bias there—we don’t know what happened to those patients.”
Patient selection at the outset remains key, Tang continued, noting that patients with secondary MR need to first be maximized on guideline-directed medical therapy, while primary MR patients need to be offered surgical care, if appropriate. “We know that with surgical mitral valve repair, if you [achieve] a near-perfect result with mild or better MR, [then] you actually restore the patient's life expectancy, whereas the problem with TEER is that if you don't get that, and you’re left with moderate or worse MR, we now have some data showing that it does not restore the patient's life expectancy and, in fact, it impacts mortality.”
From my perspective, when you do your first-time TEER, number one is you want to make sure you have mild or better MR coming out. Gilbert Tang
Following Zaid’s presenting, panelist Linda D. Gillam, MD (Morristown Medical Center, NJ), pointed out that the “huge disparity” between the rates of replacement versus repair likely speaks more to the patient substrate than to the procedures. “There were so many things there that really put them at high risk for death, so those [mortality] data I find a little bit hard to interpret,” said Gillam.
“If there are ways to improve repairability, that's probably not a bad thing,” she added. “It’s notable that the needle hasn't moved: it is still the vast majority of patients being replaced rather than repaired and I think that's telling in and of itself.”
Cardiothoracic surgeon Tsuyoshi Kaneko, MD (Barnes-Jewish Hospital, Boston, MA), commented that there is an important reminder in these data for interventional cardiologists: low-risk degenerative MR patients typically do very well with surgical MV repair. If they are treated with TEER initially, but then go on to have a replacement, that may meaningfully impact their outcomes, he said.
“But if we are able to [offer] repair, here, on these failed TEER patients, maybe that might open up the TEER option for these younger patients,” said Kaneko.
Shelley Wood was the Editor-in-Chief of TCTMD and the Editorial Director at the Cardiovascular Research Foundation (CRF) from October 2015…
Read Full BioSources
Zaid S. Mitral valve repair versus replacement after edge-to-edge transcatheter mitral repair: results from the CUTTING-EDGE registry. Presented at: TVT 2023. June 8, 2023. Phoenix, AZ.
Disclosures
- Zaid reports no relevant conflicts of interest.
- Tang reports serving as a proctor for Medtronic; a consultant for Medtronic and Abbott Structural Heart; and an advisory board member for Abbott Structural Heart and JenaValve.




Jaroslav Januska