Women Likely Not Good Targets for AAA Screening, Study Suggests
Women, who are less apt to develop AAAs, might also be more likely to suffer the consequences of added cost and overdiagnosis.
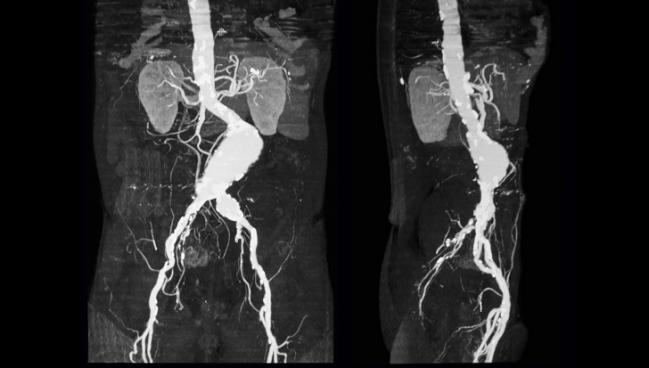
Abdominal aortic aneurysm (AAA) screening for men is standard in several countries, including the United Kingdom and Sweden. But new research suggests that women, who are less apt to develop AAAs, may not reap the same benefits from widespread screening programs, with the potential pitfalls of added cost and overdiagnosis.
AAA is four to five times more common in men than in women, and the benefits of screening women have rarely been studied. However, the effectiveness of male screenings has raised questions of whether these efforts should also extend to women.
“With long-term health-economic modelling in men suggesting that population-based screening would be cost-effective with an AAA prevalence as low as 0.35% to 0.50%, smoking now almost as common in women as in men, and with the association between smoking and AAA almost twice as strong for women compared with men, the case for AAA screening in women needs to be formally assessed,” investigators led by Michael Sweeting, PhD (University of Cambridge, England), write.
Some studies have suggested the potential benefits of screening in women, but overall the evidence has been “variable,” Janet Powell, MD, PhD (Imperial College London, England), co-author of the study, told TCTMD. “This is the first study that has actually considered harms as well as potential benefits [of screening],” she added.
In their study published in the August 11, 2018, issue of the Lancet, the researchers used data from reviews, clinical trials, and registries to create a simulated model testing the potential of AAA screening in women. What they found wasn’t encouraging.
Few Female Lives Saved
The model followed the protocol of the UK National Abdominal Aortic Aneurysm Screening Programme (NAAASP), where all men at age 65 are screened for AAA via ultrasound. Sweeting et al estimated the number of positive screenings and clinical events for 10 million women and evaluated the cost-effectiveness of these AAA screenings over time.
Using the screening and treatment protocol currently used for men in the United Kingdom, the model detected 23% more AAAs than would be detected without screening in women ages 65 to 95 years. This translated to 7% fewer deaths due to AAA in the decade after screening and 3% fewer deaths due to AAA between the ages of 65 and 95.
The researchers found that 3,900 screenings would be necessary to prevent one AAA death in this population. Comparatively, fewer than 700 men need to be invited to screening to prevent an AAA-related death.
Screening in women was also much less cost-effective than ongoing screening AAA protocols in men, with an incremental cost-effectiveness ratio (ICER) of £30,000 ($38,300) per quality-adjusted life-year (QALY) gained. For men, screening has an ICER of £7,400 ($9,450).
They were just informed that they had a ticking bomb in their stomach, but then nothing could be done about it. Minna Johansson
Applied in women, screening would result in overdiagnosis, the model suggested. One-third of cases identified as AAA likely would not have caused any symptoms or problems for the patient. Additionally, 13% of cases received surgeries that were not medically necessary.
Overdiagnosis and overtreatment are cause for concern, Minna Johansson, MD (University of Gothenburg, Sweden), told TCTMD. These screenings “find aneurysms that would never have caused any symptoms in the remaining lifetime of the person, and also you treat some of them with surgery,” said Johansson, who co-wrote an accompanying editorial with Karsten Juhl Jørgensen, MD (The Nordic Cochrane Center, Copenhagen, Denmark). Surgery, she added, can result in severe complications such as stroke.
The model also hinted at these ill effects. “For every four women who avoided an AAA death because of successful screening, one woman died due to additional elective repair,” Sweeting et al say.
Tailoring Protocol Doesn’t Help
In different calculations, the researchers adjusted the model to better target AAA in women by pushing screening to age 70 as well as decreasing the minimum aortic diameter to diagnose the condition. This math decreased AAA-related deaths by 12% for ages 70 to 80 and by 8% for ages 70 to 95. The ICER dipped to £23,000 ($29,366) and the number of screenings necessary to prevent a death also decreased to 1,800. On the flip side, overdiagnoses of AAA climbed to 55%, and nearly a quarter of elective surgeries were considered unnecessary. Additionally, for every seven women who avoided a AAA-related death due to screening, two women died during reparative surgery.
“That the healthcare system causes the death of healthy citizens by inviting them to an intervention that they have not asked for is ethically problematic,” write Johansson and Jørgensen. “It is not as simple as a matter of net benefit in terms of mortality, because it is not clear that a death saved by screening equals out a death caused by screening.”
Additionally, due to the older age of patients and likely comorbidities, there was a 55% increase in women who met criteria for elective surgery but could not undergo the procedure due to comorbidities. “They were just informed that they had a ticking bomb in their stomach, but then nothing could be done about it,” Johansson said.
While the study found that AAA screening in women would be ineffective at identifying the condition, Powell noted one potential benefit to these screenings is they could potentially evaluate overall cardiovascular health.
“If these people are picked up with small aneurysms, it means they've got some sort of cardiovascular disease,” she said. “At that point, they probably would get better treatment with statins, aspirin, and better investigation for any underlying coronary or any other cardiovascular disease.” These evaluations of general cardiovascular health occur in the men’s screening program, Powell noted, but were not evaluated in the study.
Although the findings suggest a clinical trial in women’s AAA screening would likely prove to be negative, Johansson emphasized that there are other areas in need of improvement.
Specifically, she said, improving surgical techniques for repairing these aneurysms would be helpful. “I think that there is a lot to be done with the vascular techniques in surgery in women, because women have a much higher mortality rate from elective surgery than men,” she said. “I would much rather put the research funding on that. I think that would save much more lives and be much more valuable to women with AAA.”
Johansson and colleagues have also recently studied the cost/benefit equation of AAA screening in men, concluding that this also deserves a rethink.
Lucy Hicks is the 2018 recipient of the Jason Kahn Fellowship in Medical Journalism. She is currently a master’s student…
Read Full BioSources
Sweeting MJ, Masconi KL, Jones E, et al. Analysis of clinical benefit, harms, and cost-effectiveness of screening women for abdominal aortic aneurysm. Lancet. 2018;392:487-495.
Johansson M, Jørgensen KJ. Should we screen women for abdominal aortic aneurysm? Lancet. 2018;392:454-456.
Disclosures
- Sweeting, Powell, Johansson, and Jørgensen report no relevant conflicts of interest.


Comments