CMR Could Change Diagnosis, Management of Suspected NSTEMI: OxAMI
While CMR provides “a much richer view” than angiography, the technology is, so far at least, in short supply around the world.
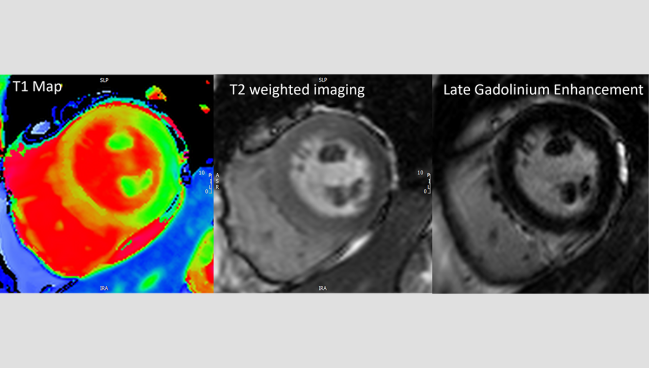
Photo Credit: Mayooran Shanmuganathan. Multiparametric CMR performed before invasive coronary angiography in a patient with suspected NSTEMI.
Using cardiac magnetic resonance (CMR) imaging to triage patients with suspected NSTEMI who are headed for invasive cardiac angiography could potentially change their diagnosis or management, according to a prospective study.
Other research has suggested that imaging, including CMR, in patients with chest pain, elevated cardiac troponins, and inconclusive ECG findings might serve as a better gatekeeper for invasive angiography, but clinical outcomes data are lacking. Moreover, despite new data emerging regarding the benefits of CMR in many arenas, most hospitals around the world don’t have access to dedicated machines.
“This is novel in the sense that MRI is confined to the stable chronic outpatient setting in most parts of the world,” lead author Mayooran Shanmuganathan, DPhil (University of Oxford, John Radcliffe Hospital, England), told TCMTD. “The UK is a pioneer in MRI, so we probably do more MRIs per capita than USA, for example, but even here, we don't do any acute scans. Very, very few. So, this is a paradigm shift if it is to happen.”
Javier Escaned, MD, PhD (Hospital Clínico San Carlos, Madrid, Spain), who commented on the study for TCTMD, said the idea of using CMR as a gatekeeper to angiography is intriguing—and that it would be “fantastic” for operators to have the extra preprocedural information provided by these scans—but he questioned its practicality. “Unfortunately, in many hospitals it is much easier to get to access to the cath lab and to have an angiogram than to access to an MRI machine,” he said, adding that the multiparametric approach the researchers used with CMR is even less widely available.
More Detailed Information on CMR
For the study, published online this week in JACC: Cardiovascular Imaging, Shanmuganathan and colleagues included 100 consecutive stable patients with suspected acute NSTEMI (mean age 62 years; 70% male) in the OxAMI study who were prospectively selected to undergo blinded CMR before proceeding with standard invasive coronary angiography in 2014-2015 and in 2018-2020. All patients presented with new chest discomfort (95%) or an equivalent symptom such as angina as well as an acute rise in high-sensitivity cardiac troponin I (hs-cTnI; median 23-fold rise above the upper limit of normal). Only 41% of patients has ischemia findings consistent with NSTEMI on ECG.
The CMR protocol included cine steady-state free precession imaging, T1 maps, bright blood T2-weighted imaging, and early as well as late gadolinium enhancement. Imaging was performed on Magnetom Tim Trio or Magnetom Verio machines (Siemens Healthcare) at a median of 33 hours after hospitalization and 4 hours before angiography.
Acute MI was confirmed by CMR in 67% of patients, including 52 subendocardial infarctions and 15 transmural MIs. Nonischemic pathologies were identified in 18% (10 myocarditis, three takotsubo cardiomyopathy, three hypertrophic or dilated cardiomyopathy, and two isolated right ventricular failure), 11% had no significant abnormalities, and 4% were inconclusive.
Compared with patients with nonischemic and normal pathologies, those with confirmed MI were more often male (81% vs 33% and 64%; P = 0.008) and had higher median elevations in hs-cTnI (43- vs ten- and fivefold above the upper limit of normal; P = 0.003). Those with normal CMR findings had higher LVEF than the other patients (61% vs 51% and 50%; P = 0.005).
After angiography, the clinical care team identified acute MI in 73% of patients (58% of whom had multivessel disease), and 85% of the acute MI patients received revascularization either by PCI (n = 56) or CABG (n = 6). Myocardial infarction with nonobstructive coronary arteries (MINOCA) was diagnosed in 27 of the 100, though ultimately only 20 were found to have the condition; among the rest, takotsubo cardiomyopathy was diagnosed in five, heart failure in one, and hypertrophic cardiomyopathy in one.
The diagnosis of MI by angiography was confirmed by CMR in only 84% of patients. For the rest, CMR identified nonischemic causes in 58% and no abnormalities in 33%. Also, 36% of patients with normal CMR findings were found to have obstructive CAD during angiography.
Diagnostic concordance regarding the infarct-related artery was achieved between CMR and angiography in 89% of patients, with CMR identifying a different culprit artery in 11%, all patients with multivessel disease.
Ultimately, the researchers calculated that if the CMR findings were made available to clinicians before invasive angiography, they could have changed the diagnosis and/or management of half of the included patients by either reclassifying the presumed NSTEMI diagnosis, identifying a different infarct-related artery, or recognizing no abnormalities.
“We believe that a CMR-first strategy is both safe and clinically feasible, as shown in our study and those by other groups,” Shanmuganathan and colleagues write. “When used as a gatekeeper to invasive coronary angiography in acute myocardial injury, it has the potential to save healthcare costs, because invasive coronary angiography may be associated with a long hospital stay and procedural complications.”
The researchers are planning a prospective randomized controlled trial designed to look at the clinical outcomes of an imaging-first strategy compared with the conventional angiogram-first strategy.
‘Much Richer View’
Although Shanmuganathan acknowledged that access to MRI will continue to be a challenge, he said NSTEMI care teams can learn from the experience of those treating stroke. “In the past, stroke teams didn't have access to MRIs and CT before they started treating a patient coming in with an acute stroke, but now it's mandatory that patients get a CT scan or an MRI scan before [treatment],” he said. “This happens 24/7 in our country now.”
Moreover, the paradigm shift the researchers are suggesting is “actually less cumbersome in the sense that NSTEMIs don't need to be done overnight,” he said. “It would be less resource-intense from that angle.”
Further, as hs-cTn assays are picking up more patients with suspected MI diagnoses, Shanmuganathan said pre-angiography imaging with CMR could potentially have even more of an impact for the growing number of MINOCA cases being caught and potentially being misdiagnosed.
“The study adds evidence to the fact that you get a much richer view [with CMR], which of course is important for patient management,” Escaned said. “And in the future, even if the patient is ischemic, it may even characterize better the type of ischemic insult that the patient had in an acute setting before PCI. And that may have prognostic implications and even perhaps implications for subsequent management of the patient.”
Escaned also spoke to the potential of CMR in the NSTEMI care pathway, in that it can identify microcirculatory disorders. That gives "one more degree of granularity in assessing a patient with NSTEMI," he said. "This, of course, would entail a more complex study, both in terms of software and in requiring resting and hyperemic image acquisition, but [this possibility] must be kept in mind when having a glimpse into the future on how comprehensive CMR interrogation can be."
Yael L. Maxwell is Senior Medical Journalist for TCTMD and Section Editor of TCTMD's Fellows Forum. She served as the inaugural…
Read Full BioSources
Shanmuganathan M, Nikolaidou C, Burrage MK, et al. Cardiovascular magnetic resonance before invasive coronary angiography in suspected non–ST-segment elevation myocardial infarction. J Am Coll Cardiol Img. 2024;Epub ahead of print.
Disclosures
- The OxAMI study is supported by the British Heart Foundation Centre of Research Excellence Oxford and the National Institute for Health Research Oxford Biomedical Research Centre.
- Shanmuganathan reports receiving funding from the Alison Brading Memorial Graduate Scholarship in Medical Science, Lady Margaret Hall, University of Oxford.
- Escaned reports no relevant conflicts of interest.





Comments